Jahrestagung der Gesellschaft für Medizinische Ausbildung
Jahrestagung der Gesellschaft für Medizinische Ausbildung
Austrian medical students’ attitudes towards end-of-life decisions: differences by year of study and implications for medical education
Text
Objective: Following the ban of the prohibition on assisted suicide in Austria in 2020, today’s medical students represent the first generation of physicians to work within a changed legal landscape. This study aimed to explore the medical students’ perspectives on the legal regulation of various end-of-life (EOL) practices. It examined their attitudes toward active euthanasia, as intentional and active acceleration or induction of death, assisted suicide, as providing a person, upon their voluntary request, with the means and information to end their own life, without direct administration by another individual, withholding or withdrawal of life-sustaining treatments, and palliative sedation, as pain-relieving treatment accepting an unintended shortening of life. Additionally, the study analyzed the influence of factors such as age, gender, year of study, and religious beliefs on opinion formation.
Methods: A cross-sectional study was conducted via an online survey among medical students at the Medical University of Vienna from May to June 2023 to explore attitudes toward EOL decisions, legal perspectives, and medical education (see figure 1 [Fig. 1]). The anonymous questionnaire included case vignettes to assess EOL decisions, questions about legal perspectives, personal reflections, decision-making responsibilities, and medical training (see figure 2 [Fig. 2]).
Figure 1: Violin plots illustrating the distribution of attitudes towards EOL decisions by religious affiliations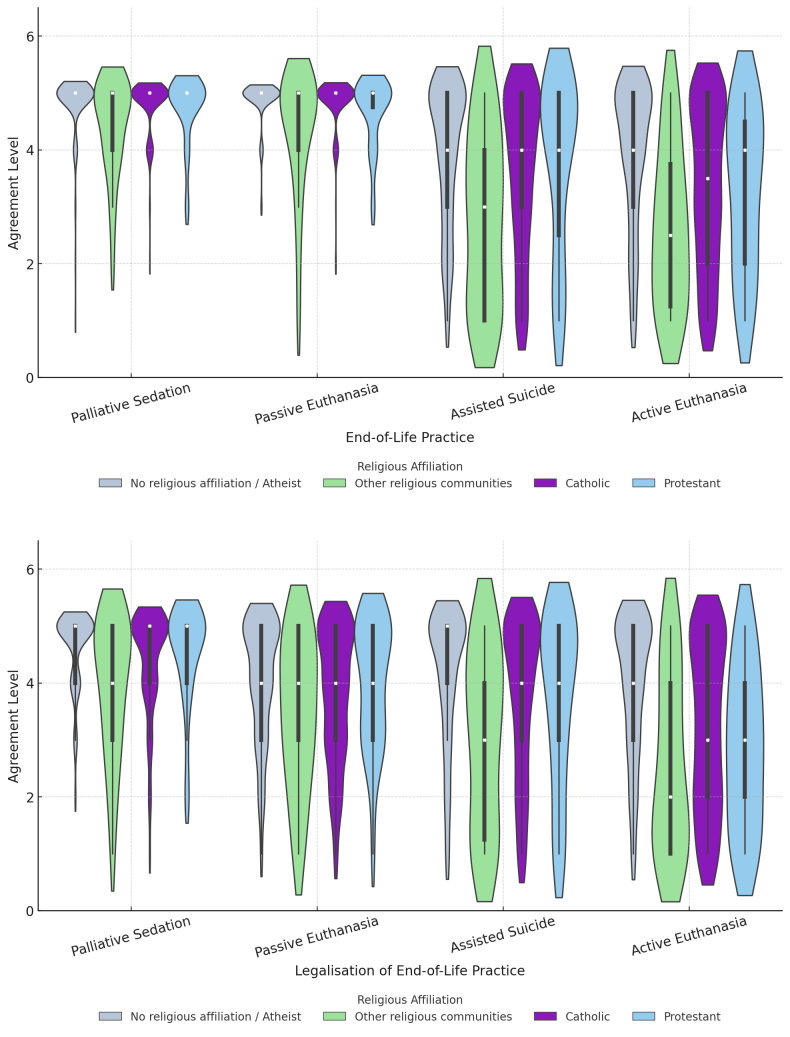
Figure 2: Spiderplots comparing agreement levels for EOL practices in hypothetical vignettes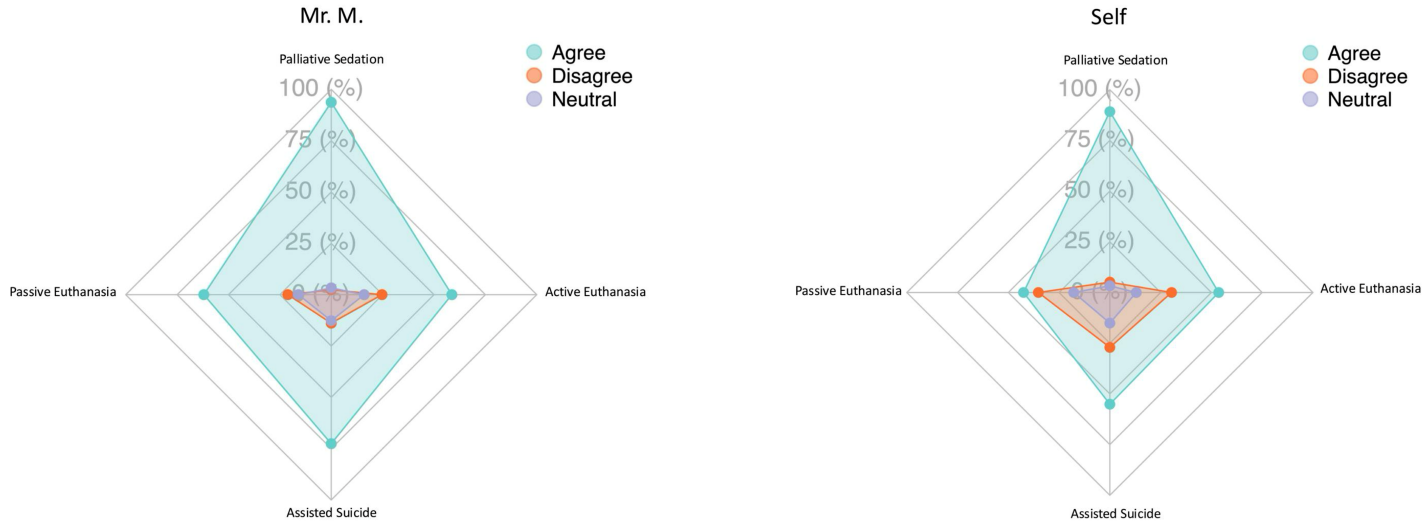
Results: The findings indicate a high level of approval for palliative sedation (94.9%) and treatment withdrawal (95.8%), while assisted suicide (63%) and active euthanasia (57.2%) were more controversially discussed. Religiosity emerged as the strongest predictor of opposition to EOL interventions, particularly regarding active euthanasia and assisted suicide. Notably, there was a discrepancy between theoretical support for EOL measures in hypothetical patient scenarios and the willingness to apply these decisions to oneself. While approximately 72% of participants supported assisted suicide for others, the approval rate dropped to 55% when considering themselves. A majority of respondents reported a lack of training in caring for terminally ill patients, with 72.9% feeling insufficiently prepared. At the same time, 93.7% expressed a desire for targeted seminars and workshops on this topic, underscoring the need for practical learning opportunities in this area.
Conclusion: The results highlight that future physicians in Austria will face complex ethical and legal challenges related to end-of-life care. The increased integration of ethical and legal aspects of EOL decision-making into medical education appears essential. Religious beliefs significantly influence attitudes; however, a majority supports the legalization of certain EOL decisions. The observed discrepancy between personal preferences and hypothetical decisions emphasizes the need for practical training and well-founded ethical reflection in the curriculum.




