Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Single-stage versus two-stage 360° fusion procedure in unstable thoracolumbar burst fractures – a bicentric trial
Text
Objectives and questions: Unstable thoracolumbar fractures often require circumferential (360°) fusion for adequate stabilization. However, debate remains over whether a single-stage or two-stage procedure yields superior outcomes. This study aims to determin wheter single-stage or two-stage 360° fusion leads to a more favourable course regarding hospital stay, operative time, blood loss, and perioperative morbidity.
Material and methods: We conducted a retrospective, bicentric analysis of 184 adult patients (Injury Severity Score ≤15) with acute unstable thoracolumbar fractures (T10–L3, AO Spine types A–C) treated at two Swiss Level I trauma centers within 6 years. All patients received 360° fusion, with first treatment within 48 hours of presentation. One center routinely performed a single-stage procedure, whereas the other favored a two-stage operation. Baseline demographics, fracture patterns, and neurological status were extracted from electronic records. The primary endpoint was total hospital length of stay. Secondary endpoints included cumulative operative time, intraoperative blood loss, and in-hospital mortality.
Results: Of 184 enrolled individuals, 104 underwent single-stage and 80 underwent two-stage surgery. Patient characteristics (median age ~42 years, male proportion ~58%, median ASA 2) were comparable between groups, although neurological deficits were significantly more prevalent in the two-stage cohort (35% vs. 6.8%). Single-stage surgery demonstrated a shorter median hospital stay of 9 days (IQR 7-11) compared to 11 days (IQR 9-14) in the two-stage group. Operative time was reduced in the single-stage approach with a median of 195 minutes (IQR 158.5-231.5) versus 230 minutes (IQR 184.8-275.3), and blood loss was lower at 500 mL (IQR 300-700) versus 750 mL (IQR 432.5-1067.5) (Figure 1 [Fig. 1]). No in-hospital deaths were observed. Subgroup analyses stratified by decompression status revealed that these differences were most pronounced among patients who underwent the additional intervention (Table 1 [Tab. 1]).
Figure 1: Main Outcomes (1-stage versus 2-stage group)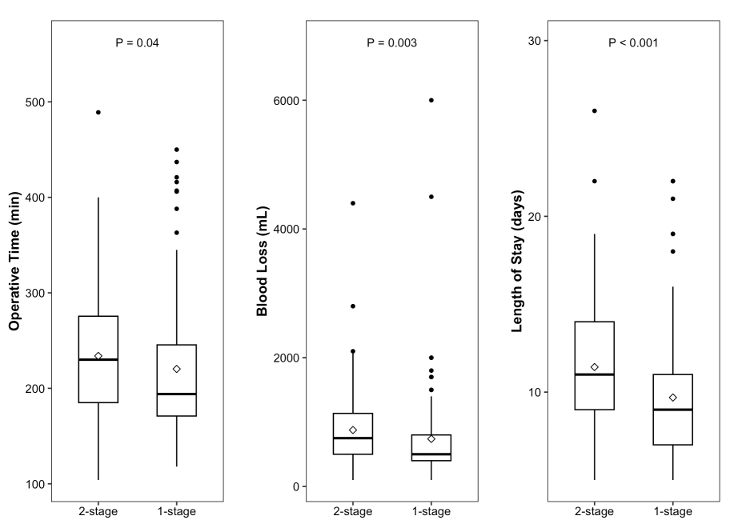
Table 1: Operative and Clinical Outcomes: Primary Analysis and Subgroup Analyses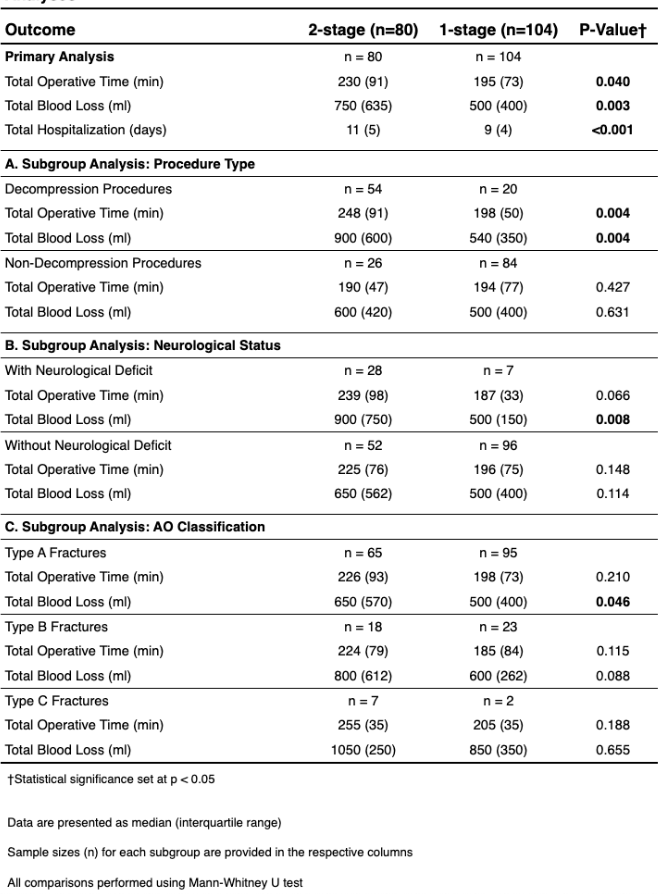
Discussion and conclusions: In this bicentric study, single-stage 360° fusion for unstable thoracolumbar fractures was associated with significantly shorter hospitalization, operative time, and blood loss compared with a two-stage approach—particularly in patients requiring decompression. Although these findings stem from retrospective, institution-specific practices, they underscore the potential advantages of a single-stage strategy. Prospective studies with standardized complication reporting, long-term follow-up, and cost analyses are warranted to confirm these benefits and guide individualized treatment decisions.




