Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Comparative analysis of medial and lateral tibial slopes in ACL-injured patients versus age- and sex-matched healthy controls
Text
Objectives: Anterior cruciate ligament (ACL) injuries are common, with posterior tibial slope influencing ACL loading and injury risk. Studies show steeper slopes in ACL-injured patients versus controls, though prior research often lacks well-matched controls for age, sex, body mass index (BMI) and injury type/severity, contributing to inconsistent findings. This study compared medial and lateral tibial slopes in ACL-injured patients and age- and sex-matched controls, with sex-specific analyses.
Methods: A prospective, cross-sectional study included 19 ACL-reconstructed (ACLR) patients who underwent ipsilateral autologous tendon replacement due to a unilateral tear [8 women, 11 men; age: 33.3±7.7 years; BMI: 24.1±2.7 kg/m²] and 19 matched controls without prior knee injuries/surgeries [8 women, 11 men; age: 33.4±7.4 years, BMI: 22.6±2.9 kg/m²]. For ACLR patients, MRI was performed 6.5±0.9 months post-surgery and 9.7±1.6 months post-injury. Additional inclusion criteria for patients were: stable/no meniscal injury, BMI <30 kg/m2, and no prior lower limb joint injuries/surgeries.
MRI scans were acquired using a 3T clinical MRI scanner (Magnetom Vida, Siemens) with an 18-channel knee coil and a 3D T2 SPACE imaging sequence (voxel size: 0.6×0.6×0.6 mm³, flip angle: 120°, repetition time: 1,000 ms, echo time: 108 ms).
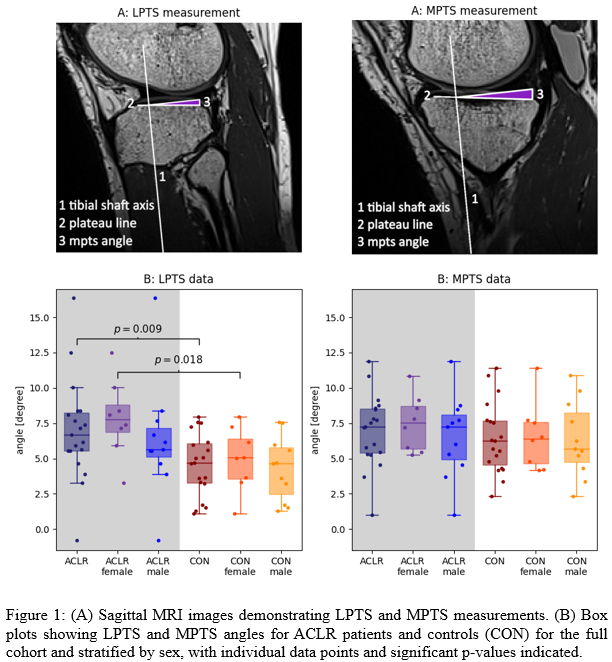
Tibial slope was measured manually. The central sagittal slice was selected based on posterior cruciate ligament attachment, intercondylar eminence visibility, and tibial cortex shape. The tibial shaft axis was defined using two circles: one touching the anterior, posterior, and superior cortical edges, and another placed distally, contacting anterior and posterior cortices. Medial posterior tibial slope (MPTS) and lateral posterior tibial slope (LPTS) were measured as the angles between the tibial shaft axis and plateau lines (Figure 1A [Abb. 1]). Measurements were taken three times and averaged.
Descriptive statistics were computed as means ± standard deviations. Group differences in MPTS and LPTS were assessed with unpaired t-tests or Wilcoxon-Mann-Whitney tests for the full sample, and then by sex (α=0.05).
Results: MPTS did not differ between ACLR patients (6.9°±2.4°) and controls (6.4°±2.4°, p=0.267). LPTS was significantly steeper in ACLR patients (7.0°±3.5°) than controls (4.6°±2.1°, p=0.009), with significance noted only in females (7.9°±2.6° vs. 4.9°±2.1°, p=0.018), and not in males (p>0.05) (Figure 1B [Abb. 1]).
Conclusions: A steeper LPTS is associated with ACL injury, particularly in females, suggesting sex-specific risk factors. This may predispose individuals to ACL injury by increasing anterior tibial translation and ACL strain. The findings underscore the need for individualized prevention and treatment strategies and highlight LPTS as a relevant anatomical factor in ACL pathology.