70. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V.
70. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V.
NutriScoPe – lessons learned from distributed analysis in nutrition science
Text
Introduction: Malnutrition is a frequently underdiagnosed condition among hospitalized patients in Germany, despite its strong association with adverse clinical outcomes such as prolonged hospitalisation or mortality [1]. Untreated malnutrition also increases healthcare costs, underscoring the practical relevance of standardized detection. As indicated by studies such as EFFORT [2], the implementation of early nutritional therapies following structured screening has been demonstrated to yield favourable outcomes and to mitigate the risk of complications. Recent international studies highlight how Clinical Decision Support Systems (CDSS) and federated learning significantly enhance diagnosis accuracy in healthcare [3].
The NutriScoPe project addresses this issue through a retrospective, data-driven study evaluating the prevalence, detection, and treatment of malnutrition using structured nutritional screening methods. The project leverages the Nutritional Risk Screening 2002 (NRS) tool. It aims to (1) assess the impact of NRS on the detection and treatment of malnutrition and (2) identify subgroups of patients with increased malnutrition risk.
Methods: NutriScoPe uses routine data from patients who are treated between 2013 and 2023 at University of Leipzig Medical Center (UKL) and University Hospital Jena (UKJ). Clinical data is requested using the Research Data Portal for Health (FDPG) and provided by Data Integration Centers (DIC) available in both hospitals. Data analysis is distributedly executed, i.e., clinical data never leaves institutional borders and no data requester has direct access to this data. By contrast, all data is analyzed by R-based pipelines which are packaged into Docker images and deployed on-site. Aggregated, non-identifiable results are returned to the data requester for interpretation.
We started with data quality assessments using the Greifswald Data Quality Concept [4] implemented in the R package dataquieR. Statistical analysis includes descriptive statistics, correlation analyses, and outcome comparisons (e.g., length of hospital stay, re-admission). Additionally, unsupervised learning techniques (e.g., k-means, hierarchical clustering) are applied to discover different risk levels.
Results: Both cohorts at UKL were descriptively analyzed with regard to baseline characteristics. Initial analyses indicate that consistent screening enabled the identification of patients with risk of malnutrition (see table 1 [Tab. 1]). Cluster analyses show promise in identifying clinically meaningful subgroups with differing needs and risks. NutriScoPe provides insights into challenges and benefits of analyzing clinical data in a distributed manner.
Table 1: Number of patients and patients with NRS mainscreening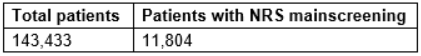
Discussion and conclusion: While full evaluation is still ongoing, NutriScoPe serves as a blueprint for data-driven studies. First findings of patients at nutritional risk with this analysis support the potential value of automated diagnosis in improving clinical nutrition care of patients, whose malnutrition would persist unseen without screening. Heterogeneous data formats (e.g., diagnosis coding) limited interoperability despite FHIR usage. Therefore, more homogenization is necessary. Developing analytical pipelines requires a playground with similar data as provided by DIC, while containerization has proven reproducibility and scalability. However, the project underlines the importance of aligning clinical relevance with robust technical infrastructures, and the lessons learned will inform both future research and the development of artificial intelligence-based clinical decision support systems.
The authors declare that they have no competing interests.
The authors declare that a positive ethics committee vote has been obtained.
References
[1] Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr. 2006;25(4):563–72. DOI: 10.1016/j.clnu.2006.03.005[2] Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet. 2019;393(10188):2312–21. DOI: 10.1016/S0140-6736(18)32776-4
[3] SK, Navyav K, Seth K, Sharma D, Singh SK, Patil S. Enhancing Clinical Decision Support Systems with Big Data and AI in Medical Informatics. Semin Med Writ Educ. 2024;3:503. DOI: 10.56294/mw2024503
[4] Schmidt CO, Struckmann S, Enzenbach C, et al. Facilitating harmonized data quality assessments: a data quality framework for observational health research data collections with software implementations in R. BMC Med Res Methodol. 2021;21:63. DOI: 10.1186/s12874-021-01252-7




