German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Clinical and radiological long-term results after permanent epiphysiodesis around the knee for correction of leg-length discrepancies
Text
Objectives and questions: Permanent epiphysiodesis (pED) is an established procedure for correcting leg length discrepancies (LLD) greater than 2 cm in skeletally immature patients. pED according to Phemister (Figure 1 [Abb. 1]) has shown satisfactory results in this regard, but has over time been widely abandoned in favor of less invasive procedures. Nevertheless, various modern pED techniques are based on the Phemister principle. However, there are currently no long-term studies on the effects of Phemister pED on knee joint morphology and potential early-onset osteoarthritis.
Figure 1: Phemister epiphysiodesis. A rectangular block of cortical bone containing the peripheral physis with adjacent meta-epiphyseal bone is extracted, then reinserted after 180-degree-rotation. Thus, premature epiphysio-diaphyseal fusion is induced. The procedure is executed on the lateral and medial aspect of the distal femur and/or proximal tibia.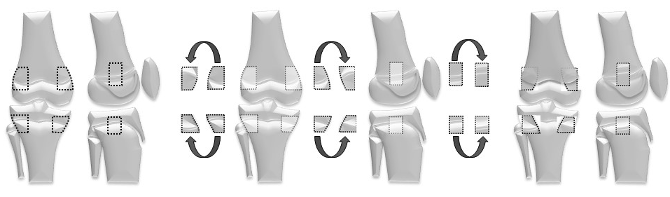
Material and methods: Long-term results of 20 patients who underwent Phemister pED for treatment of LLD between 1980–2006 were retrospectively evaluated, and the results were compared with an age-matched untreated control group of 10 patients. The clinical and radiological analysis included the evaluation of LLD, mechanical axis deviation (MAD), periarticular joint angles, central knee joint anatomy, and osteoarthritis grading. Patient-reported outcomes were assessed using the Oxford Knee Score (OKS), EQ-5D-3L, and the Knee Injury and Osteoarthritis Outcome Score (KOOS).
Results: The mean follow-up was 37 years (28–40). The mean LLD was 2.8 cm (1.3–4.3) preoperatively and 1.1 cm (0.1–2.3) at the last follow-up. A LLD greater than 1 cm was present in 55% of patients at the time of the last examination. No significant differences were observed between the patients and the control group for either the periarticular or intra-articular joint angles. Initial gonarthrosis (Kellgren-Lawrence grade 1) was found in two patients, but none in the control group. Patient-reported outcomes showed worse results for patients regarding the OKS and quality of life compared to the control group, while no relevant differences were found for the KOOS.
Discussion and conclusions: Phemister pED shows satisfactory results regarding the correction of LLD without evidence of an increased rate of secondary frontal axis deviations, intra-articular deformities, or early osteoarthrosis of the knee joint. However, compared to the untreated control group, patients reported more knee joint complaints and slightly reduced joint function. Although the traditional Phemister pED is rarely used today, the study results justify the continued use of pED procedures based on the Phemister principle without increased risk of long-term sequelae.




