German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Proximal femoral replacement in revision total hip arthroplasty for severe femoral bone loss: A 20-year experience
Text
Objectives and questions: Proximal femoral replacement (PFR) is a salvage procedure in revision total hip arthroplasty (THA) for extensive femoral bone loss. This study aimed to evaluate implant survivorship and clinical outcomes of PFR for non-oncologic indications at midterm follow-up.
Material and methods: Sixty-one consecutive PFRs for non-oncologic indications performed between 2000 and 2022 at a single academic institution were reviewed. The most common indication was periprosthetic fracture and reimplantation after periprosthetic joint infection (each 33%), followed by aseptic loosening (31%) and dislocation (3%). Femoral bone loss was severe in all patients, with 49% Paprosky type IIIb defects and 51% Paprosky type IV defects. The majority of PFRs were cemented (98%). Constrained liners were used in 26 patients (43%), while standard head-liner constructs were used in 25 patients (41%) and dual-mobility constructs in 10 patients (16%). Outcomes of interest included implant survivorship, mortality rates, and clinical outcomes. Revision, reoperation, dislocation, and aseptic failures were considered as time-to-event outcomes, and were analyzed using the cumulative incidence function, accounting for the competing risk of death. The mean patient age was 77 years, with 67% being female. Mean follow-up was 5 years.
Results: The 5-year cumulative incidence of any revision and any revision of the femoral component was 24% and 8%, respectively (Figure 1 [Fig. 1]). The 5-year cumulative incidence of any reoperation was 30%. Dislocation was the most common reason for revision (n=8), with a 5-year cumulative incidence of 15%, followed by periprosthetic joint infection (n=4), periprosthetic fracture (n=2), and aseptic loosening (n=1). Among the 10 patients who dislocated, 8 patients (80%) underwent revision to a constrained liner at a mean of 2 years. The 5-year cumulative incidence of revision for aseptic loosening of the PFR was 2%. The 2- and 5-year mortality rates were 14% and 42%, respectively.
Figure 1: Cumulative incidence of revision with death as a competing risk factor.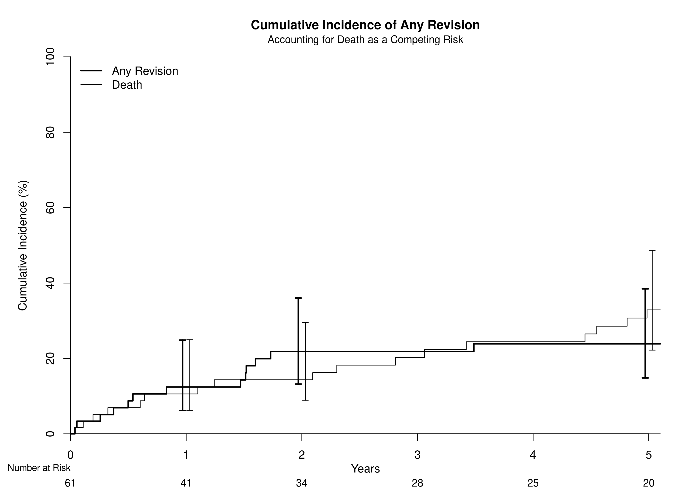
Discussion and conclusions: In this complex cohort of 61 PFRs for non-oncologic revision THA, revision and reoperation rates were modest, with dislocation as the predominant failure mode. Although aseptic loosening was rare, mortality remained high.




