German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Clinical efficacy of collum femoris preserving prosthesis in femoral head replacement for elderly patients with femoral neck fractures
Text
Objectives and questions: To evaluate the clinical efficacy of Collum Femoris Preserving (CFP) prosthesis in femoral head replacement for elderly patients with femoral neck fractures.
Material and methods: A retrospective study was conducted on elderly patients who underwent femoral head replacement for femoral neck fractures between June 1, 2011, and June 1, 2013. Demographic and clinical data, including gender, age, Garden classification, prosthesis type, operative time, intraoperative blood loss, length of hospital stay, postoperative bilateral femoral offset, follow-up duration, Harris Hip Score (HHS), and Oxford Hip Score (OHS) at the final follow-up, were collected. Patients were selected based on predefined inclusion and exclusion criteria, with those receiving the CFP prosthesis assigned to the observation group and those receiving conventional biological prostheses to the control group. Comparative analysis of the aforementioned variables was performed to assess the recovery of hip joint function.
Results: A total of 64 patients were included, with a mean follow-up period of 83.6 ± 6.9 months (range: 70–94 months). The observation group comprised 36 patients, while the control group included 28 patients. No significant differences were observed between two groups in baseline characteristics such as age, gender distribution, classification, length of hospital stay, or follow-up duration (P > 0.05). However, the observation group exhibited a significantly shorter operative time (76.4 ± 16.8 vs. 85.4 ± 11.7 minutes, P = 0.01) and reduced intraoperative blood loss (355.6 ± 164.7 vs. 432.1 ± 121.9 mL, P = 0.04). The absolute differences in postoperative bilateral femoral offset were 4.2 ± 0.9 mm in the observation group and 3.9 ± 0.9 mm in the control group, with no statistically significant difference (P = 0.198). At the final follow-up, no significant differences were observed in functional outcomes, with mean HHS values of 80.5 ± 5.7 and 80.6 ± 5.7 (P = 0.94) and mean OHS values of 13.7 ± 2.8 and 14.6 ± 3.9 (P = 0.28) in the observation and control groups, respectively.
Discussion and conclusions: The CFP prosthesis demonstrates comparable long-term hip joint functional outcomes to conventional biological prostheses in elderly patients with femoral neck fractures at 7–8 years postoperatively. The CFP prosthesis, however, offers advantages in terms of reduced intraoperative blood loss and shorter operative time. Thus, the CFP prosthesis is a safe and effective option for femoral head replacement in this patient population.
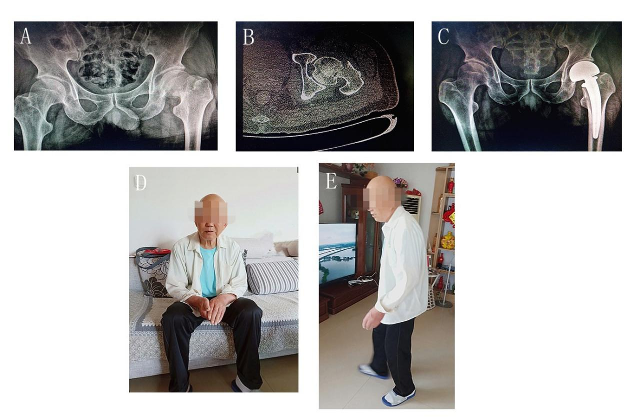
Figure 1 [Abb. 1]
Figure 1: A typical case of femoral head replacement using a CFP prosthesis.