German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
The aging spine: Assessing the interplay between disc degeneration and disability
Text
Objectives and questions: The relationship between degenerative changes in the lumbar spine and chronic low back pain (cLBP) remains controversial. While lumbar degeneration is more common in symptomatic patients, its role in pain and disability is described inconsistently. We hypothesize that the association between spinal degeneration and pain, as well as disability, is more pronounced in younger patients, necessitating an age-specific analysis.
Material and methods: This study prospectively enrolled patients aged 18 to 64 with and without cLBP. Exclusion criteria included malignant diseases, spinal infections, and vertebral fractures. Spinal degeneration was assessed via MRI using the Pfirrmann classification for disc degeneration and the Fujiwara classification for facet joint degeneration. A combined lumbar score was calculated for both degeneration types. Multivariable logistic regression models analysed the association between spinal degeneration and cLBP, while linear regression models examined the relationship with SF-36 physical (PCS) and mental (MCS) component scores, with age used interaction term. All models were adjusted for sex, BMI, physical activity, and smoking as potential confounders. Statistical significance was set at p < 0.05.
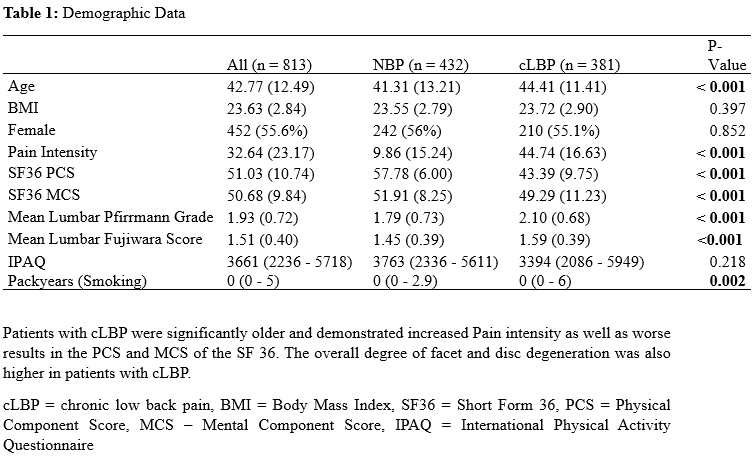
Results: A total of 813 participants were analysed (mean age: 42.7 years, SD 12.5; median BMI: 23.6, SD 2.8). Among them, 294 patients (46.8%) reported cLBP. (Table 1 [Tab. 1]). Logistic regression showed that combined lumbar disc and facet degeneration had a stronger association with cLBP than individual levels (p < 0.001). Interaction analyses indicated a decline in the strength of this association with age (disc: OR: 0.96, 95% CI: 0.93 - 0.98, p < 0.001; facet: OR: 0.94, 95% CI: 0.91 - 0.98, p = 0.003) (Table 2 [Tab. 2]). Subgroup analysis showed similar lumbar disc degeneration effects across sexes, but a stronger facet degeneration association in females. The SF-36 PCS also correlated significantly with lumbar disc degeneration (β: -10.20, 95% CI: -15.30 - -5.10, p < 0.001) and facet degeneration (β: -13.52, 95% CI: -22.16 - -4.87, p = 0.002), also showing a significant interaction with age (Figure 1 [Fig. 1]), while SF-36 MCS showed no significant associations.
Discussion and conclusions: This study demonstrates an age dependent and significant association between lumbar degeneration, cLBP and physical disability. This indicates that younger patients with spinal degeneration are more likely to experience cLBP with the association weakening with age. These findings may explain the varying results in the literature and emphasize the importance of age specific considerations in cLBP evaluation and management, potentially helping to guide targeted treatment strategies.