German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Biomechanical stability optimization in preoperative planning for tibal plateau fractures
Text
Objectives and questions: Complex tibial plateau fractures pose significant challenges in orthopedic surgery due to their intricate nature and potential complications [1]. Plate and screw fixation is a common surgical approach, but the optimal positioning of plates and screws remains a topic of debate.
Finite Element Modelling (FEM) provides a quantitative method for evaluating the biomechanical performance of various osteosynthesis constructs under physiological loading conditions [2].
This study aims to improve conventional preoperative planning by using FEM as a measure for assessing and optimizing biomechanical performance. It is hypothesized that optimized osteosynthesis configurations provide greater stability than standard approaches.
Material and methods: Schatzker IV fractures with lateral depression were induced in six left human lower extremity cadaveric specimens (Rimasys, Germany). They underwent a computed tomography (CT) scan, after which the proximal tibia fragments were segmented and realigned to achieve anatomic fracture reduction.
All fracture fixations were planned with a medial variable angle locking plate (Pangea, Stryker, Switzerland). Initial implant configurations were based on standard surgical planning by a fellowship trained surgeon. Then, each case underwent an iterative process to optimize plate and screw positions by means of FEM. To evaluate the stability of the osteosynthesis constructs, initial and final configurations were biomechanically simulated using Abaqus (Simulia, Dassault Systèmes, France). Knee joint reaction forces were scaled according to patient weight and patient-specific Hounsfield-Unit-derived bone material properties were applied to the 3D model.
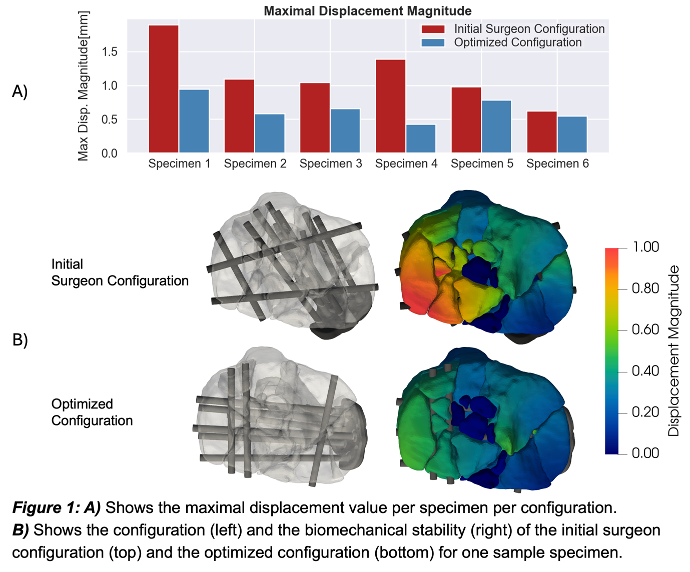
Results: The mean maximal displacement magnitude for the initial surgeon configuration was 1.17 mm (SD = 0.43 mm) while in the optimized configuration, it was 0.66 mm (SD = 0.19 mm) which corresponds to a mean relative reduction of 39.25%. This represents a significant reduction in maximal displacement (p = 0.01) achieved with no significant change in number of screws used (MInitial = 11, SD = 1.27, MOptimized = 11, SD = 0.89, p = 0.50).
Discussion and conclusions: Optimizing plate and screw positioning significantly reduced displacement compared to conventional planning, especially in initially unstable constructs.
The improvement in stability was particularly pronounced in constructs where the initial configuration showed large displacements.
Hence, patient-specific FEM provides valuable insights into how plate positioning affects fracture stability, which may guide orthopedic surgeons towards optimized plate placement strategies.
Figure 1 [Fig. 1]