German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Greater meniscal extrusion and inferior patient reported outcomes after medial compared to lateral meniscal allograft transplantation
Text
Objectives and questions: Meniscal extrusion is common after meniscal allograft transplantation (MAT). However, there is no consensus regarding normal extent of extrusion in different weight-bearing states using ultrasound and how it correlates with clinical outcome and joint degeneration. This study aimed to compare meniscal extrusion after MAT on ultrasound and evaluate its correlation with patient-reported outcome measures (PROMs).
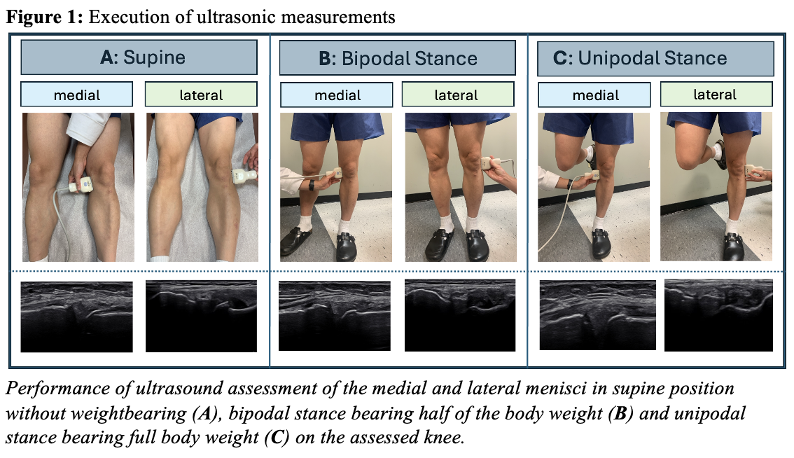
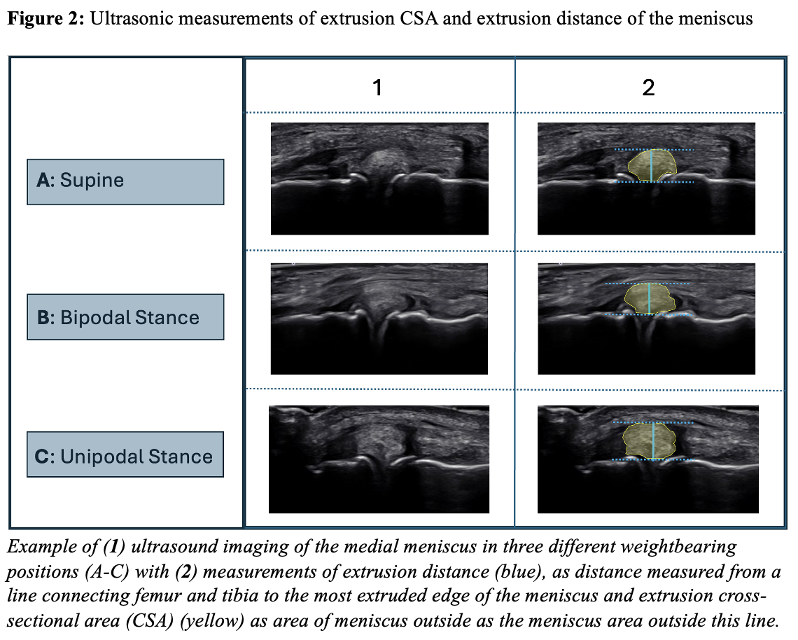
Material and methods: Patients who underwent MAT with minimum 1-year follow-up were included. Exclusion criteria included untreated cartilage injury grade IV at the time of MAT, subsequent MAT resection, and subsequent total knee arthroplasty. All ultrasound measurements were taken in supine position, bipodal, and unipodal stance. Ultrasound was used to measure cross-sectional area (CSA) and distance of extrusion of the meniscus and compared to the equivalent contralateral meniscus to assess side-to-side (STS) differences. Measurements were assessed anterior to the lateral collateral ligament for the lateral meniscus and parallel to the medial collateral ligament for the medial meniscus. Extrusion distance was measured from a line connecting femur and tibia to the most extruded meniscus edge, while extrusion CSA was defined as the meniscus area outside this line. Additionally, bilateral radiographs and PROMs were obtained at the latest follow-up.
Results: Thirty-three patients (average age at MAT 29.8 ± 10.5 years; 33% females; 33% lateral MAT) were assessed via ultrasound at a mean follow-up of 10.0 ± 5.4 years after MAT. Mean IKDC SKF was 64.1 ± 18.9. In the overall cohort, ultrasound revealed greater extrusion CSA of the transplanted meniscus compared to contralateral in all positions. There were no significant differences in baseline demographics between the medial and lateral MAT groups. Extrusion CSA STS difference was greater in the medial MAT group than the lateral MAT group in all positions (bipodal/unipodal/supine, 27.6 vs. 11.8 / 27.4 vs. 9.7 / 25.8 vs. 9.2 mm2, respectively, p<0.05). Similarily, the STS difference in extrusion distance was greater in the medial MAT group in two positions. The International Knee Documentation Committee Subjective Knee Form (IKDC SKF) was significantly inferior in the medial MAT group compared to the lateral MAT group (57.2 vs. 78.1, respectively, p<0.05).
Discussion and conclusions: The findings of this study indicate that medial MAT results in more pronounced meniscal extrusion than lateral MAT as measured by ultrasound in a long-term follow-up and is also associated with inferior PROs. Further research is required to evaluate long-term effects of meniscal extrusion on radiological outcomes.
Figure 1 [Fig. 1]
Figure 2 [Fig. 2]