German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
An intraindividual comparison of center-center versus center-posterior blade positioning using the femoral neck system in unstable posterior tilted pauwels II femoral neck fractures – a biomechanical cadaver study
Text
Objectives and questions: Internal fixation of femoral neck fractures (NF) remains associated with high revision rates. Notably, increased fracture displacement correlates with an elevated risk of implant failure. Specifically, a posterior tilt exceeding 20° – measured as the angle between the mid femoral collum line and the radial collum line on lateral radiographs — is linked to a higher reoperation rate. The Femoral Neck System (FNS) has proven to be a reliable implant in treatment of NF. A center-center blade position is the recommended implant placement, but biomechanical cadaver studies comparing different blade positions are lacking. We hypothesized that a center-posterior positioning in patients with a higher dorsal posterior tilt due to a posterior comminution zone may be superior to the recommended center-center positioning.
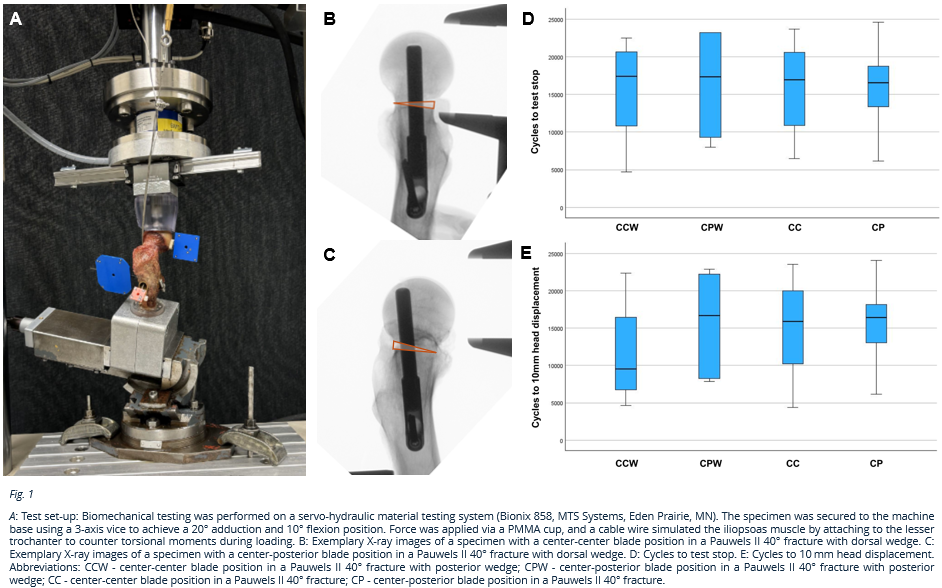
Material and methods: 24 paired fresh-frozen human femora (12 female donors) were used, with bone mineral density (BMD) determined for each donor. Based on BMD, donors were allocated to one of two fracture configurations: a standard Pauwels II 40° fracture or a Pauwels II 40° fracture with an additional 10° posterior wedge defect. For each donor, the same fracture configuration was simulated bilaterally using standardized osteotomies. The implant blade position was varied between the left and right femora; one side received a center-center (CC) position while the contralateral side received a center-posterior (CP) position. Radiographic imaging was performed to confirm accurate reduction and implant positioning. Biomechanical testing was performed with specimens positioned in 20° adduction and 10° flexion, with simulated iliopsoas muscle tension. Incremental cyclic loading was applied until construct failure occurred. Interfragmentary movements between the femoral head and shaft were quantified using optical motion tracking, and the data were statistically analyzed with significance set at p<0.05.
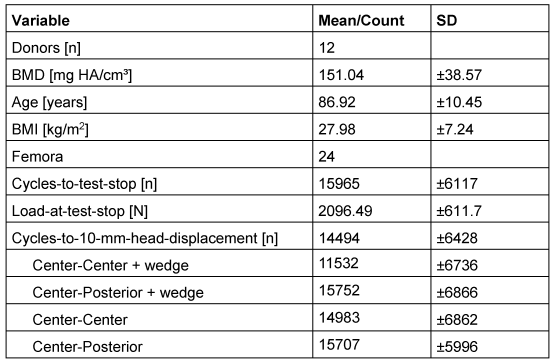
Results: The groups did not differ in mean age, BMD, or BMI. Mean construct failure occurred after 15,965±6,117 cycles at 2,096.5±611.7N. Cycles-to-10-mm-head-displacement averaged 14,494±6427 cycles (Table 1). Pairwise comparisons showed no statistically significant differences regarding blade position.
Discussion and conclusions: The variation in blade positioning from center-center to center-posterior did not prove superior in this study. The center-center position remains the preferred standard alongside achieving anatomical reduction.
Table 1 [Tab. 1]
Figure 1 [Abb. 1]