German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Biomechanical analysis of surgical technique on distal femoral replacement implant performance
Text
Objectives and questions: When distal femoral resection is required due to a bone tumor, Distal Femur Replacement (DFR) can restore joint functionality. Implant stability depends on the structural integrity of the residual femur and the efficiency of the bone-implant interface in transmitting and distributing loads. Both cemented and press-fit fixation techniques are available. In press-fit solutions, the presence of a stem and/or collar at the bone-implant interface may enhance stability.
This study aims to provide surgical guidelines and evaluate the biomechanical performance of cemented and press-fit DFR solutions by analyzing and comparing bone stress distribution and implant stability.
Material and methods: A validated finite element model was developed using the cortical bone geometry of a standard femur. DFR implant components (stem, collar, and shaft) were modeled based on geometries provided by the manufacturer.
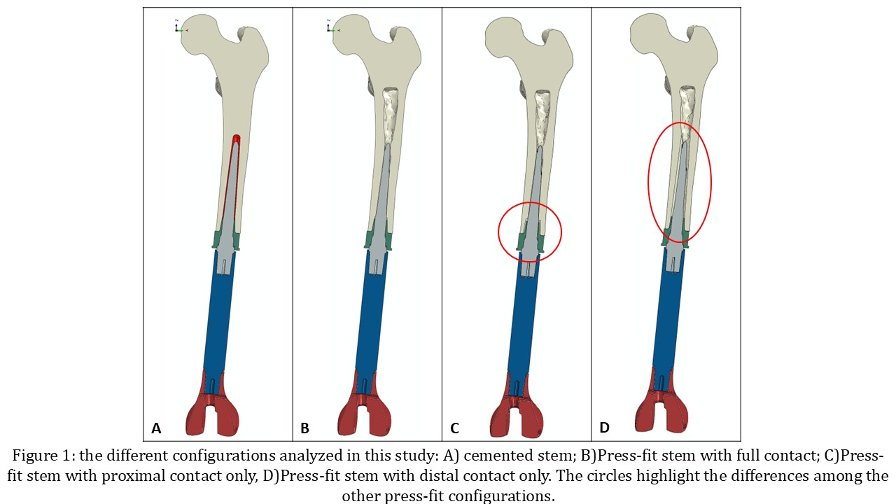
Four fixation scenarios were examined (Figure 1 [Abb. 1]):
Cemented stem;
Press-fit stem with full contact (both proximal and distal);
Press-fit stem with proximal contact only (no collar contact);
Press-fit stem with distal contact only (no stem contact).
Consistent with previous studies, simulations were performed at 0° knee flexion (with a 1,000 N force applied along the femoral mechanical axis) and at 90° knee flexion (with a 200 N force applied along the anterior direction). In both cases, the femoral head was considered fixed. DFR performance across configurations was evaluated by assessing implant stability and bone stress distribution in several regions of interest.
Results: The fixation technique significantly influenced stress distribution and implant stability in both the bone and the implant.
At both 0° and 90° flexion, cemented fixation exhibited the lowest stress levels in both the distal and proximal bone regions. Full press-fit configurations and no-collar press-fit solutions showed higher but comparable stress values. However, the absence of stem contact led to a higher concentration of bone stress in the collar region, increasing the risk of bone fracture.
Regarding implant stability, full press-fit configurations exhibited the least micromotion, followed by collar-less press-fit and cemented solutions (all below 20 microns). The configuration lacking stem contact resulted in significantly higher implant micromotion (exceeding 100 microns) and should be avoided.
Discussion and conclusions: While press-fit solutions provide favorable implant stability when the stem is properly engaged, they are highly sensitive to surgical positioning and the bone-implant contact interface. Given these challenges, cemented fixation emerges as the optimal compromise, balancing surgical feasibility and bone stress management in DFR procedures.