German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
The role of Bone Morphogenetic Protein (BMP) in accelerating fracture healing and functional recovery in HIV-infected patients
Text
Objectives and questions: Individuals living with HIV have a significantly higher risk of fractures compared to the general population. Optimizing treatment strategies for these patients is critical to improving outcomes. This study investigates the clinical application of Bone Morphogenetic Protein (BMP) in the surgical treatment of HIV-infected patients with traumatic fractures, aiming to provide evidence-based recommendations for enhancing treatment protocols.
Material and methods: A retrospective cohort study was conducted on HIV-positive patients with fractures who underwent surgical treatment at Zhongnan Hospital of Wuhan University between January 2013 and December 2021. A total of 53 eligible patients were included and divided into two groups: the BMP group (n = 28) and the control group (n = 25). Surgical site infections were managed using the Vacuum Sealing Drainage (VSD) technique.
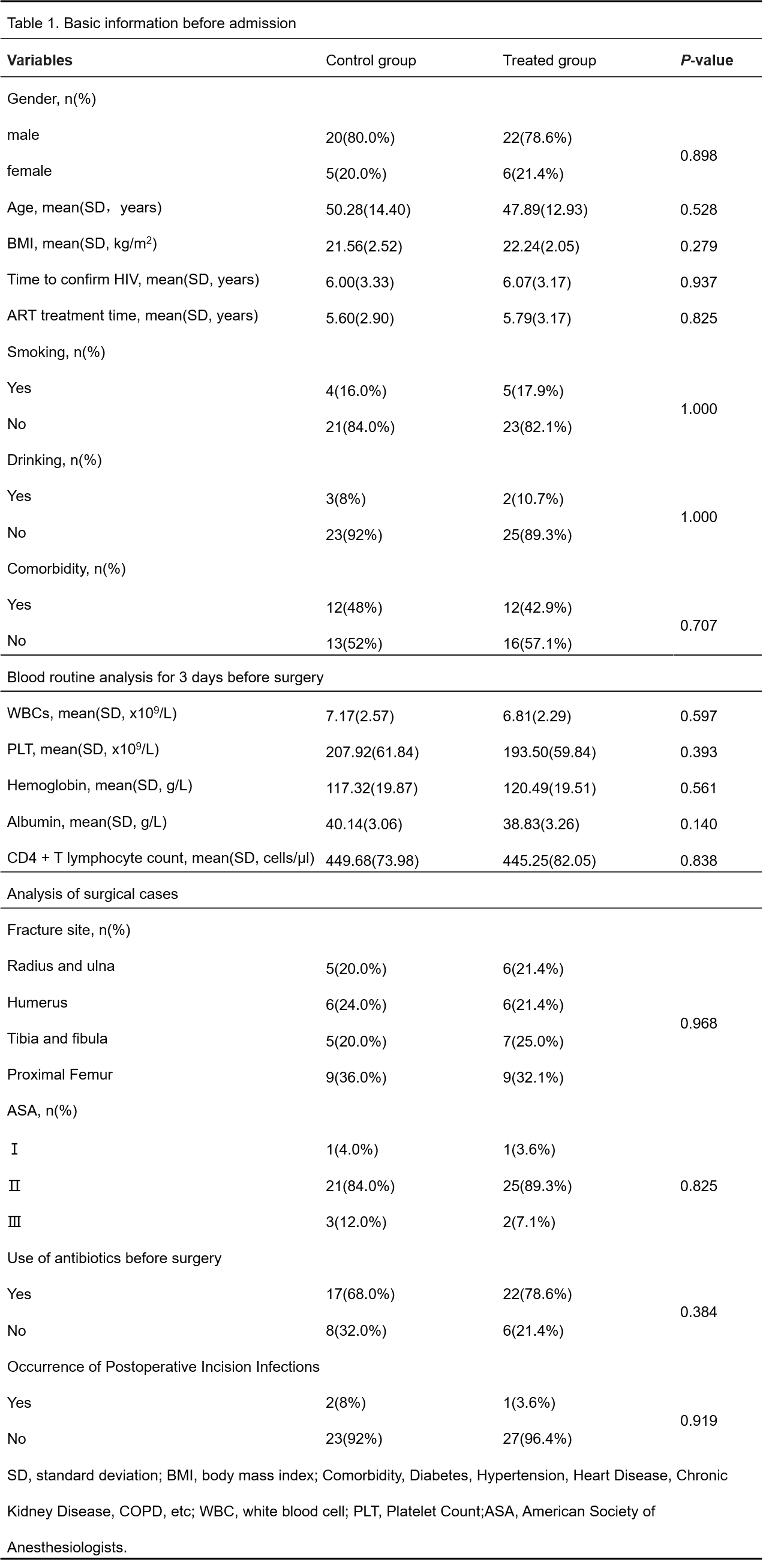
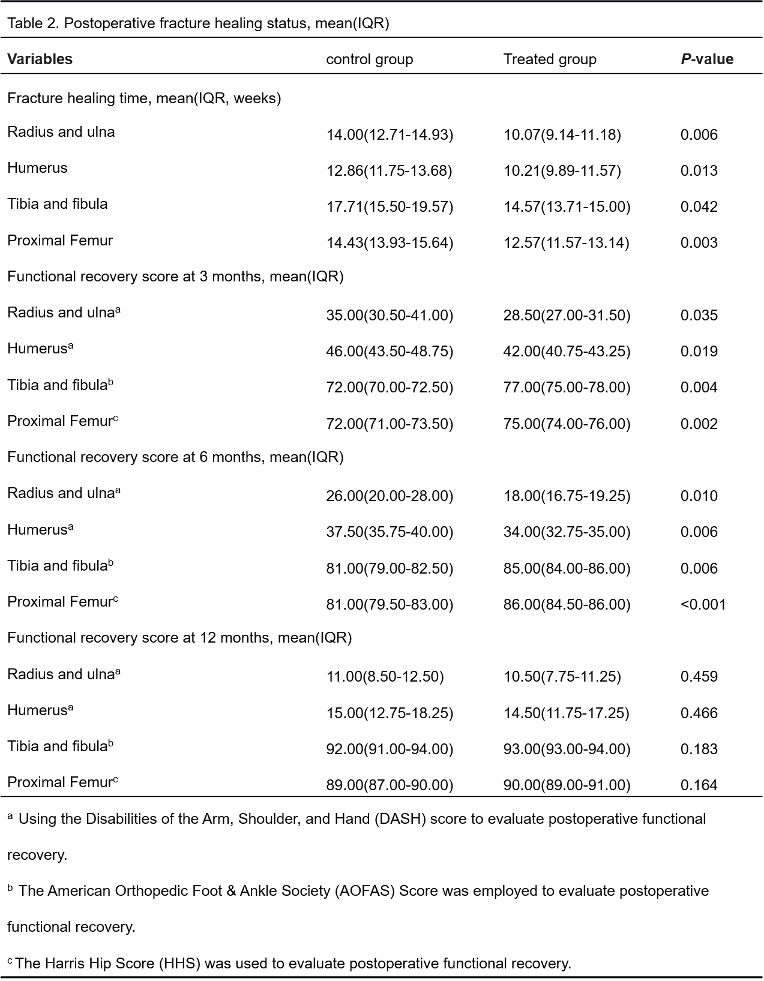
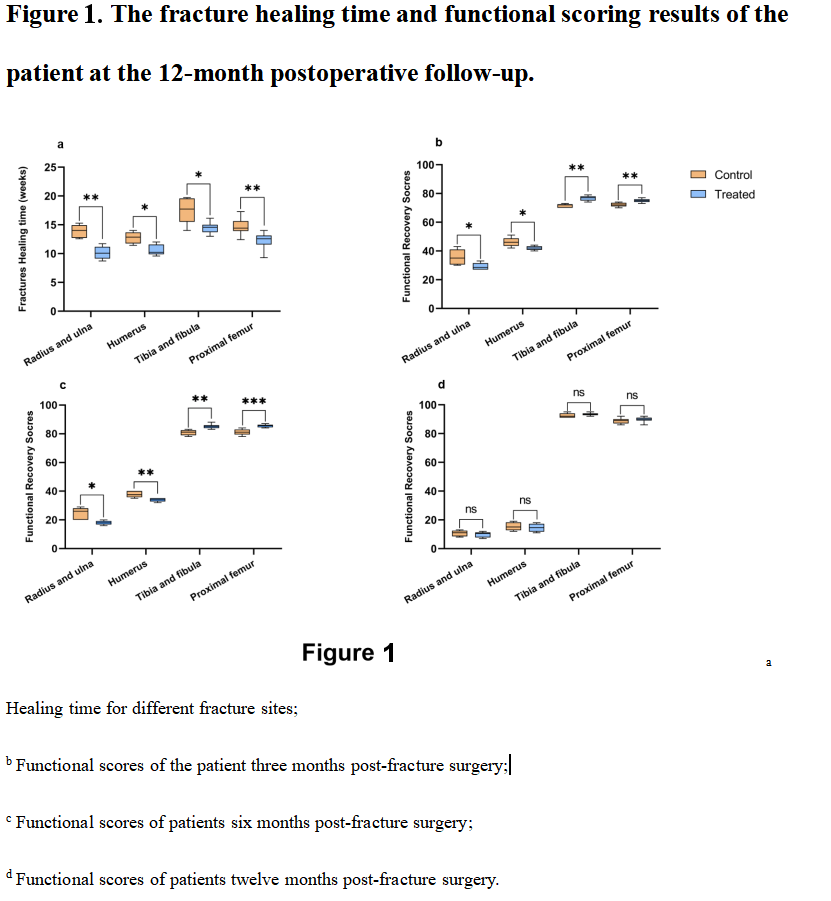
Results: The analysis revealed no significant differences in the baseline characteristics of the two patient groups (P > 0.05), Table 1 [Tab. 1]. At 12 months postoperatively, the experimental group showed significantly shorter median fracture healing times compared to the control group. The median healing times in the experimental group were as follows: radius and ulna, 10.07 weeks (IQR 9.14–11.18); humerus, 10.21 weeks (IQR 9.89–11.57); tibia and fibula, 14.57 weeks (IQR 13.71–15.00); and femur, 12.57 weeks (IQR 11.57–13.14). In contrast, the median healing times in the control group were: radius and ulna, 14.00 weeks (IQR 12.71–14.93); humerus, 12.86 weeks (IQR 11.75–13.68); tibia and fibula, 17.71 weeks (IQR 15.50–19.57); and femur, 14.43 weeks (IQR 13.93–15.64). All differences were statistically significant (P < 0.05). Functional recovery scores at 3 and 6 months were also significantly better in the experimental group across all fracture types (P < 0.05), Table 2 [Tab. 2], Figure 1 [Fig. 1]. During the study period, one case of postoperative incision infection occurred in the experimental group, while there were two cases in the control group. There was no significant difference in the incidence of incision infections between the two groups (P > 0.05). All infected patients achieved successful healing following vacuum-assisted closure (VSD) treatment.
Discussion and conclusions: BMP application significantly shortens fracture healing times in HIV-infected patients and promotes early functional recovery. Additionally, the VSD technique proved effective in managing postoperative incision infections, successfully controlling infections and reducing the risk of iatrogenic exposure for healthcare workers. These results provide valuable insights and references for optimizing the surgical treatment of fractures in HIV-infected patient.