German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Association of paraspinal muscle atrophy and lumbar spinal mobility
Text
Objectives and questions: Muscle atrophy is recognized as a contributor to spinal dysfunction. While previous research has linked paraspinal muscle degeneration to pain, its association with spinal mobility remains unclear. Given the critical role of lumbar function in daily function, we aim to investigate this relationship.
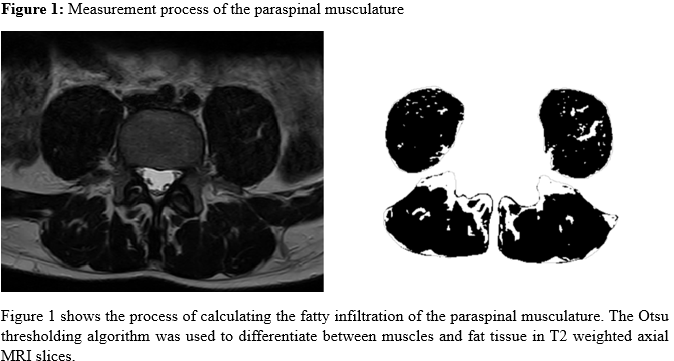
Material and methods: Participants aged 18 to 64 with and without chronic low back pain (cLBP) were prospectively enrolled from the general population. Patients with specific LBP were excluded. Paraspinal atrophy was assessed by measuring the fat infiltration (FI) of the multifidus (MF), and erector spinae (ES) at each lumbar level using T2-weighted axial MRI sequences (Figure 1 [Abb. 1]). Spinal mobility was evaluated in a standing position, measuring maximum flexion/extension of the lumbar spine with a gyroscopic device. The association between muscle FI and spinal mobility was analysed via linear regression, adjusted for age, sex, Body Mass Index, disc degeneration, physical activity and current pain intensity on the numeric analogue scale.
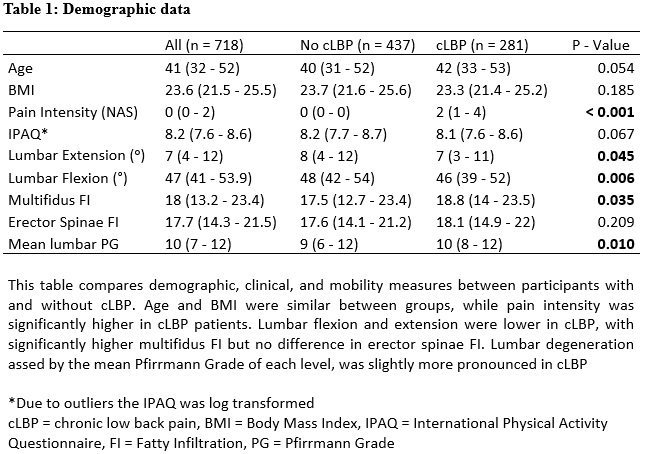
Results: A total of 718 participants (61.9% female) with a median age of 41 years (IQR: 32–52) were included. Demographic variables are shown in Table 1 [Tab. 1]. Multivariable analysis showed a significant association between FI in both the multifidus (MF) and erector spinae (ES) muscles and reduced lumbar mobility. Specifically, greater FI in the MF was linked to decreased flexion (β: -0.48, p < 0.001) and extension (β: -0.11, p = 0.033). Similarly, higher FI in the ES was associated with reduced flexion (β: -0.44, p < 0.001) and extension (β: -0.16, p = 0.007). Subgroup analysis by pain status revealed that FI was significantly associated with lumbar flexion in both cLBP and non-cLBP participants (p < 0.01). However, the association with extension was only significant in those without cLBP (p < 0.05). The effect of ES FI on mobility was weaker in the cLBP group, as indicated by a lower partial eta² value (1.3 vs. 3.4 in the non-cLBP group).
Discussion and conclusions: This study highlights the association of paraspinal muscle atrophy and spinal mobility. Interestingly the impact was stronger on flexion, likely due to its stabilizing role despite the ES being a primary extensor. The weaker association with extension in cLBP suggests that pain-related adaptations and neuromuscular changes may play a larger role in this subgroup than structural changes alone. These results indicate the rehabilitation should not only focus on passive flexibility improvement but also on extensor function to improve lumbar mobility.