German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Paraspinal muscle atrophy and lumbar disc degeneration: Independent or interconnected processes?
Text
Objectives and questions: Paraspinal muscle atrophy and disc degeneration are hallmarks of spinal aging, yet their interaction remains unclear. To better define their interplay, this study aims to investigate the association between paraspinal muscle atrophy and lumbar disc degeneration in individuals with and without chronic low back pain (cLBP).
Material and methods: Participants aged 18 to 64 with and without chronic low back pain (cLBP) were prospectively enrolled from the general population. Paraspinal muscle atrophy was assessed on T2-weighted axial MRI by measuring fat infiltration (FI) and functional cross-sectional area (fCSA) of the multifidus (MF) and erector spinae (ES) at each lumbar level. FI and fCSA values were averaged across all lumbar levels to reflect overall muscle condition. Lumbar disc degeneration was classified according to the Pfirrmann Classification at each level, and a mean lumbar value was calculated. The association between muscle and disc degeneration was analyzed in participants with and without cLBP using multivariable linear regression models, adjusted for age, sex, Body Mass Index (BMI), physical activity, measured by the International Physical Activity Questionnaire (IPAQ), and smoking.
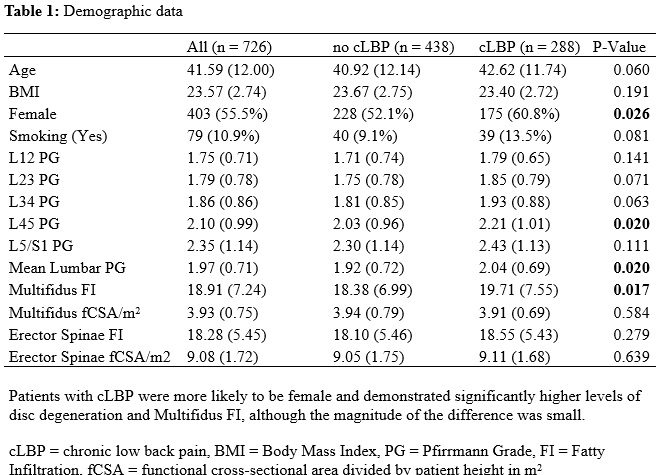
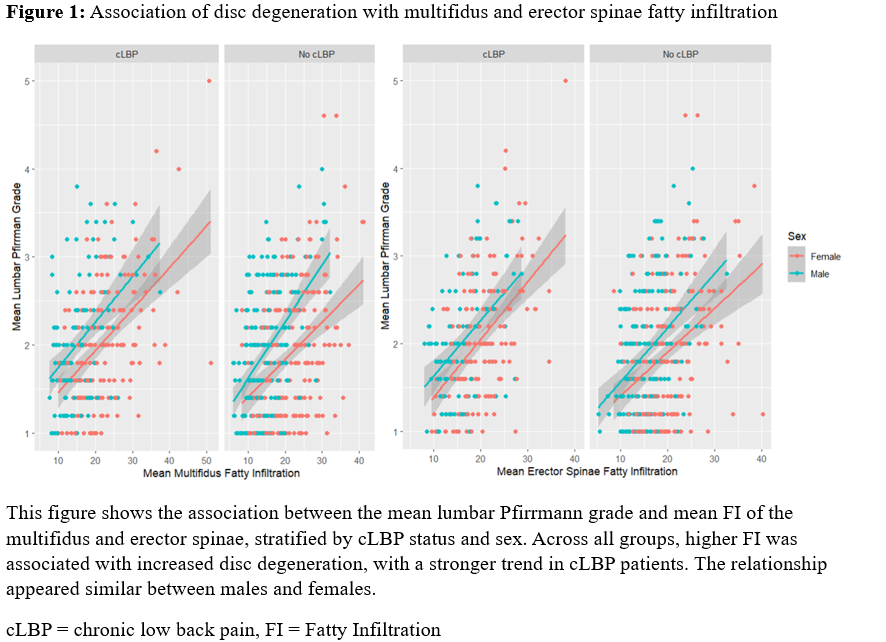
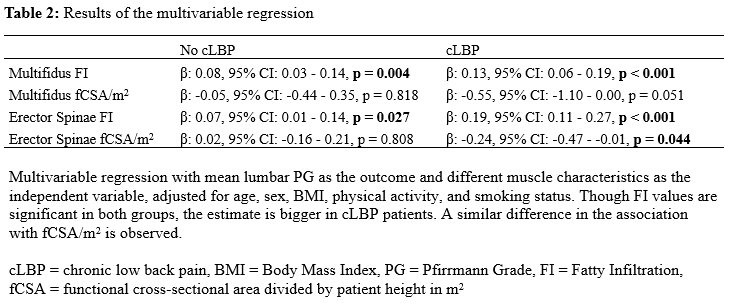
Results: A total of 726 participants (55.5% female). Patients characteristics are summarized in Table 1 [Tab. 1]. The unadjusted association between disc degeneration and FI is shown in Figure 1 [Abb. 1]. In the multivariable analysis, FI of the MF and ES were associated with increased levels of disc degeneration in both groups (p < 0.05). However, the association was stronger in the cLBP group (Table 2 [Tab. 2]). In contrast to the no cLBP group, a significant negative association between disc degeneration and fCSA of the erector spinae was observed in the cLBP group (β: -0.24, 95% CI: -0.47 to -0.01, p = 0.044), with a similar, though not significant trend, for MF fCSA (β: -0.55, 95% CI: -1.10 to 0.00, p = 0.051).
Discussion and conclusions: This study confirms an independent association between paraspinal muscle atrophy and lumbar disc degeneration, with a stronger association in cLBP patients. While FI was significantly linked to disc degeneration in both groups, the association was more pronounced than the fCSA, highlighting its potential as a key marker of muscle degeneration. These findings suggest that assessing FI may provide valuable insights into spinal degeneration and warrant further investigation into its role in disease progression and potential therapeutic targets.