German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Predictive value of the preoperative CCI for perioperative total hip arthroplasty complications
Text
Objectives and questions: Primary total hip arthroplasty is often indicated for conditions such as osteoarthritis, rheumatoid arthritis, and avascular necrosis. While the procedure generally has favorable outcomes, the risk of complications remains a concern for both surgeons and patients.
The Clavien-Dindo classification provides a standardized method to grade complications. It categorizes surgical complications into five grades based on the required treatment, from Grade I (Minor complications not requiring intervention), over Grade II (requiring pharmacological treatment or transfusions), over Grade III (Complications requiring surgical intervention), Grade IV (Life-threatening complications requiring intensive care) and Grade V (Death).
The Charlson Comorbidity Index (CCI) is a scoring system that assesses the burden of comorbid diseases on a patient’s overall health. It assigns a score based on the presence of various chronic conditions, with higher scores indicating greater comorbidity burden.
This study examines the relationship between the CCI and postoperative complications classified by Clavien-Dindo in the context of primary THA.
Material and methods: A retrospective study was conducted involving patients who underwent total hip arthroplasty procedures between 2021 and 2024 at an academic institution. Preoperative CCI scores were calculated for each patient, encompassing a range of comorbid conditions and their severity. Perioperative complications were documented and classified using the Clavien-Dindo classification, ranging from grade I to grade V.
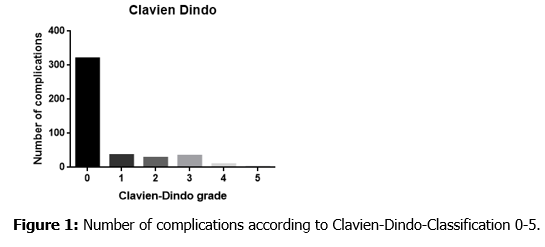
Results: The study included 424 patients with a median CCI score of 1 (Mean=1.3; SD=1.6 range 0-8). Perioperative complications (≥ Grade I) occurred in 17% (72/424) of patients, with 76.4% (55/72) classified as non-surgical and 23.6% (17/72) as surgical complications.
Higher preoperative CCI scores were associated with an increased risk of perioperative complications, (Pearson’s r = 0.47, p < 0.0001). Additionaly, higher Clavien-Dindo grades were associated with age (r=0.15; p<0.002), ASA score (r=0.23; p<0.0001), anticoagulants (r=0.2; p< 0.0001), preoperative Hemoglobin levels (r=-0.28; p<0.0001) and estimated intraooperative blood loss (r=0.23; p< 0.0001) and surgery duration (r=0.26; p<0.0001).
Discussion and conclusions: The preoperative CCI is a valuable predictor of perioperative complications classified by the Clavien-Dindo system. Higher CCI scores are correlated with increased risk and severity of complications. Understanding the predictive value of the CCI can aid surgeons in preoperative planning and patient counseling. By identifying patients at higher risk for complications, healthcare providers can implement targeted strategies to mitigate these risks. This study underscores the importance of comprehensive preoperative assessment using the CCI to identify high-risk patients, allowing for tailored perioperative management strategies to mitigate potential complications.
Figure 1 [Abb. 1]
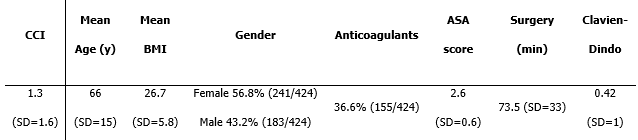
Table 1 [Tab. 1]
Table 1: Pateint demographics CCI, Charlson Comorbidity Index; y, years; BMI, body mass index in (Kg/m2); ASA, American Society of Anesthesiologists