German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Machine learning-driven gait classification in individuals with anterior cruciate ligament reconstruction
Text
Objectives: Anterior cruciate ligament (ACL) ruptures often lead to gait abnormalities, and while ACL reconstruction (ACLR) is a common treatment, it may not fully restore normal biomechanics. Machine learning (ML) provides a robust method for analyzing multidimensional gait data, extracting features from complex waveforms to identify abnormalities. This study developed an ML-based biomechanical score to classify pathological gait in ACLR patients, supporting early detection of altered biomechanics that may compromise joint integrity.
Methods: Twenty-one patients who underwent ipsilateral four-strand semitendinosus (single-bundle) ACLR (3.3 ± 1.5 months after unilateral ACL rupture) [9 women, 12 men; age 34.0 ± 8.1 years; body mass index (BMI) 24.3 ± 2.8 kg/m2] and 79 healthy controls [37 women, 42 men; age 33.3 ± 8.2 years; BMI 23.6 ± 2.9 kg/m2] completed self-paced treadmill walking (ACLR: 6.6 ± 0.9 months post-surgery). Three-dimensional marker trajectories and ground reaction forces were recorded using a 14-camera system and two force plates (GRAIL, Motek). Gait cycle-normalized waveforms were averaged for knee flexion-extension (FE) angles and moments, and abduction-adduction (AA) moments. A multistep approach yielded the biomechanical score: hierarchical clustering (single linkage) to exclude control outliers; statistical parametric mapping (SPM) to identify group-specific regions of interest (ROIs); principal component analysis (PCA) to reduce ROIs to a two-dimensional (2D) space; determination of group centers (ACLR vs. healthy); score computation as the distance of individual points along a vector between the group centers, scaled to one standard deviation (SD) of healthy gait; selection of classification threshold using Youden’s J statistic to maximize sensitivity and specificity; and classification performance evaluation via area under the receiver operating characteristic curve (AUC).
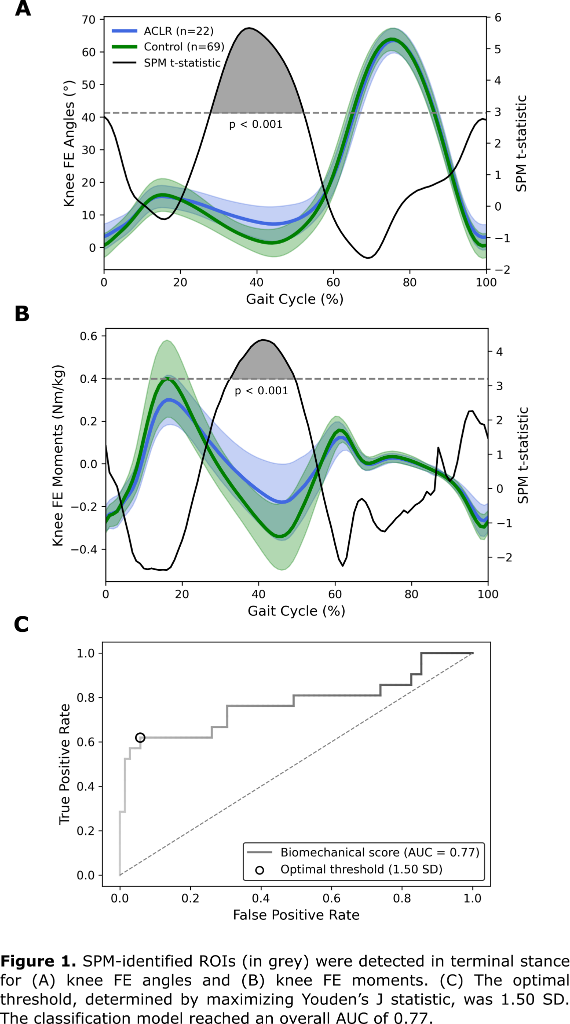
Results: Hierarchical clustering excluded ten controls as outliers. SPM identified ROIs during terminal stance for knee FE angles (28–52% of the gait cycle) and moments (33–49% of the gait cycle), but none for AA moments (Figure 1 [Abb. 1]). In the PCA-reduced 2D space, the ACLR group center was 1.37 SD from the control group, reflecting deviation from healthy gait. The optimal classification threshold was 1.50 SD. The biomechanical score achieved an AUC of 0.77.
Conclusions: The biomechanical score detected pathological gait in ACLR patients with moderate classification performance (AUC = 0.77). Despite limitations, including restriction to sagittal and frontal plane knee joint data and a small ACLR sample, it represents a valuable tool for early detection of abnormal gait after ACLR. Consequently, it may help guide interventions to prevent joint deterioration from abnormal biomechanics.