70. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V.
70. Jahrestagung der Deutschen Gesellschaft für Medizinische Informatik, Biometrie und Epidemiologie e.V.
Bridging Technology and Organizational Change: A Context-Sensitive Strategy for Mandatory HIS Implementation in a University Hospital
Text
Introduction: The implementation of hospital information system (HIS) is often framed as a technological upgrade, yet it fundamentally alters clinical workflows and organizational culture – particularly in mandatory settings. At a large German university hospital, a vendor based HIS will be introduced by 2028, affecting more than 23,000 staff across 100+ specialist departments. Evidence shows that mandatory implementations may provoke resistance and tensions if contextual factors are not adequately addressed [1], [2]. This study protocol adapts the Basel Approach for Contextual Analysis in Implementation Science (BANANA) [3] to systematically identify and address these factors during the pre-implementation phase.
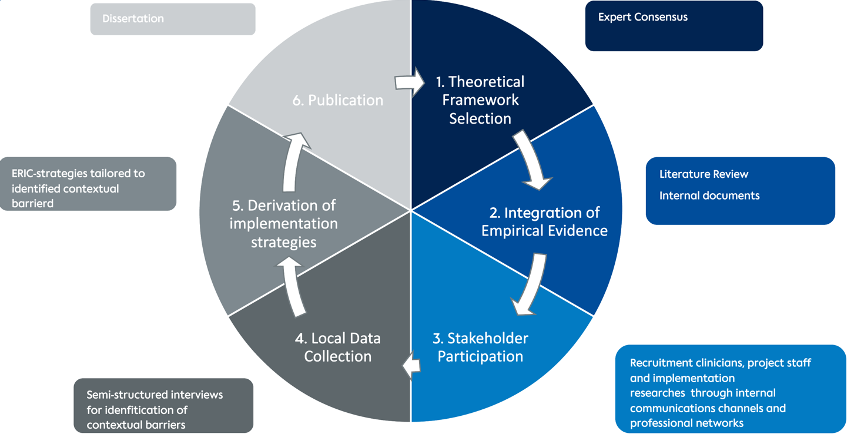
Methods: The study follows a multi-method design based on BANANA’s six-step framework [3].
- A theoretical framework will be selected through expert consensus among implementation researchers.
- A hermeneutic literature review will be conducted alongside insights from internal project documents.
- Stakeholders – including clinicians, project staff, and implementation experts – will be recruited through internal communication channels and professional networks.
- Semi-structured interviews will explore perceived contextual barriers and facilitators.
- Based on the interview findings, tailored implementation strategies will be selected using the Expert Recommendations for Implementing Change (ERIC) [4].
- The contextual analysis process and its findings will be reported transparently in line with implementation science standards.
Figure 1 [Abb. 1]
Results: The study is expected to classify key contextual barriers and produce stakeholder-informed strategies tailored to the hospital’s environment. These outcomes will form the basis of an implementation guide that addresses the complexities of a mandatory HIS rollout in a university hospital.
Discussion: This research is situated at the intersection of medical informatics and implementation science, addressing a highly complex, mandatory digital transformation at a German university hospital. Such transformations require not only interoperability and standardization of data flows across departments but also deep integration into clinical routines. These technical challenges – ranging from infrastructure compatibility to interface usability and system reliability – can significantly disrupt clinical processes if not managed thoughtfully. Despite the technological sophistication of the HIS, resistance, low adoption, and workflow misalignment remain persistent risks, particularly in mandatory implementation settings [1], [2]. This is precisely where implementation science adds value: by providing structured methodologies to understand context, engage stakeholders, and tailor implementation strategies to real-world conditions. Using the BANANA approach for contextual analysis and drawing upon prominent implementation frameworks and tools, this project contributes a context-sensitive, user-informed guide for implementation within a complex environment [5], [3], [4]. Ultimately, the integration of implementation science into medical informatics is not just beneficial – it is essential. Only through interdisciplinary collaboration can we ensure that complex digital health technologies are not only technically sound but also usable, accepted, and effective in practice.
Conclusion: Operationalizing BANANA [3] in a large clinical setting offers a structured approach to early-stage contextual analysis. By identifying barriers and co-designing solutions with stakeholders, this study aims to reduce resistance and support successful HIS adoption. The results may inform other large-scale digital health implementations.
The authors declare that they have no competing interests.
The authors declare that a positive ethics committee vote has been obtained.
Literatur
[1] Boonstra A, Versluis A, Vos JF. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res. 2014 Sep 4;14(1):370. DOI: 10.1186/1472-6963-14-370[2] Brown SA, Massey AP, Montoya-weiss MM, Burkman JR. Do I really have to? User acceptance of mandated technology. Eur J Inf Syst. 2002 Sep;11(4):283-95.
[3] Mielke J, Leppla L, Valenta S, Zullig LL, Zúñiga F, Staudacher S, et al. Unraveling implementation context: the Basel Approach for coNtextual ANAlysis (BANANA) in implementation science and its application in the SMILe project. Implement Sci Commun. 2022 Oct 1;3(1):102. DOI: 10.1186/s43058-022-00354-7
[4] Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015 Feb 12;10(1):21. DOI: 10.1186/s13012-015-0209-1.
[5] Damschroder LJ, Reardon CM, Widerquist MA, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022 Oct 29;17(1):75. DOI: 10.1186/s13012-022-01245-0