- Conferences Overview
- Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
- Pain and pain management following manual versus robotic assisted unicondylar knee arthroplasty
German Congress of Orthopaedics and Traumatology (DKOU 2025)
28.-31.10.2025
Berlin
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Pain and pain management following manual versus robotic assisted unicondylar knee arthroplasty
Text
Objectives and questions: The use of robotic technology for unicondylar knee arthroplasty (UKA) has increased. However, its influence on short-term outcomes compared to manual techniques remains uncertain. Therefore we studied whether robotic assistance independently reduces hospitalization, pain, and analgesic use after UKA.
Material and methods: We identified 1369 opioid-naïve patients who underwent medial, unilateral UKA at a single institution between 2019 and 2023 (417 manual and 952 robotic). In-hospital and 6-week Numeric pain rating Scale (NRS) pain scores, in-hospital use of non-opioid analgesics and anti-emetics, length of stay, and opioid consumption collected. Opioids prescribed and consumed were converted to morphine milligram equivalents (MMEs). Outcome variables were compared between manual and robotic cases with multivariable linear regression adjusting for age, BMI, sex, Charlson Comorbidity Index, ASA Class, race, marital status, smoking status, insurance type, and use of nerve block.
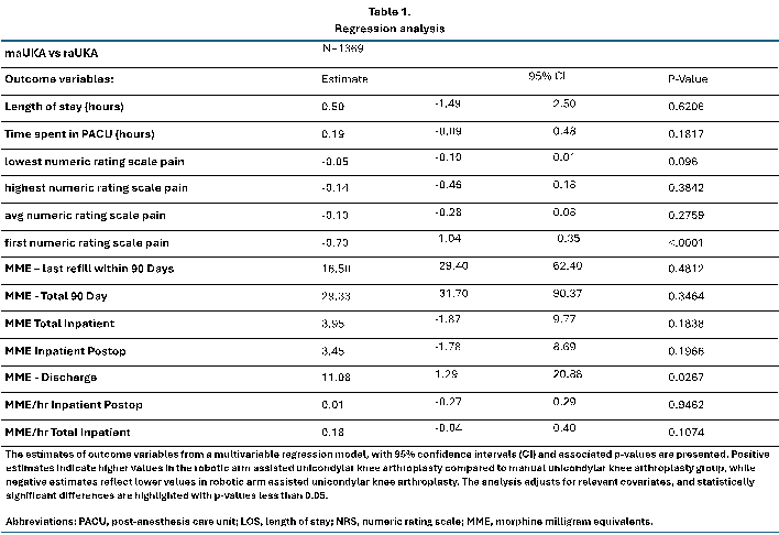
Results: Patients who underwent robotic UKA had higher pain scores reported in the recovery room (Estimate -0.7, p<0.001); however, there was no difference in the minimum, maximum, or average pain score reported during hospitalization. Robotic UKA was associated with lower ketorolac utilization (Estimate 0.29; p=0.011). Manual and robotic UKA patients had no significant difference in length of stay (22.8 and 20.4 hours respectively; p=0.094). There was no statitistically significant difference in in-patient opioid consumption (47.42 and 40.01 MMEs; p=0.143 respectively 2.26 and 2.14 MMEs/hour; p=0.564); no difference in the amount prescribed at discharge (295 and 291 MMEs; p=0.599); refilled within the first 90 days (27.5 and 26.8 MMEs; p=0.380); and in the total 90-day (899 and 851 MMEs; p=0.787) opioid utilization (Table 1 [Tab. 1]).
Discussion and conclusions: Robotic assistance in UKA was not independently associated with improvements in hospitalization time, pain, or opioid use within 90 postoperative days. Further exploration of potential short and long-term benefits to robotic UKA may help identify clinical advantages to justify the added expense.