- Conferences Overview
- Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
- Minimal changes in patella height after aseptic revision from unicompartmental to total knee arthroplasty
German Congress of Orthopaedics and Traumatology (DKOU 2025)
28.-31.10.2025
Berlin
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Minimal changes in patella height after aseptic revision from unicompartmental to total knee arthroplasty
Text
Objectives and questions: If revision of a unicompartmental knee arthroplasty (UKA) is required, converting it to a total knee arthroplasty (TKA) remains the favored approach. However, worse functional outcomes after revision from UKA to TKA are reported compared to primary TKAs. One potential driver may be a decline in patella height, limiting knee flexion, and increasing patellofemoral stress. Therefore, the aim of this study was to assess whether the patella height changes after revision from UKA to TKA.
Material and methods: We retrospectively analyzed 128 aseptic UKA to TKA revisions between 2015 and 2022 at a single medical center. True lateral radiographs were obtained before revision (T1), one week after revision (T2), and at the last follow-up (T3). Two orthopedic surgeons independently measured the modified Insall-Salvati ratio (mISR) at each time point. The mean age was 67 years, 67% were female, and the mean BMI was 32 kg/m². The mean follow-up was 1.5 years.
Results: The mean mISR was 1.59 ± 0.3 at T1, and 1.58 ± 0.2 at T2, respectively, with no significant difference between T1 and T2 (p=0.72, Figure 1 [Abb. 1]). At T3 the mean mISR was 1.52 ± 0.2, with no significant difference to T2 (p=0.57, Figure 1). Overall, 24 patients (19%) experienced a patellar tendon shortening of ≥10%. For T3 measurements obtained beyond 6 months postoperatively the mISR decreased by 3% compared to T2 (p=0.03).
Figure 1: Comparison of the modified Insall-Salvati Ratio (mISR) immediately before Revision from unicompartmental (UKA) to total knee arthroplasty (TKA) (T1), One Week after Revision from UKA to TKA (T2), and at last Follow-up after Revision from UKA to TKA (T3). 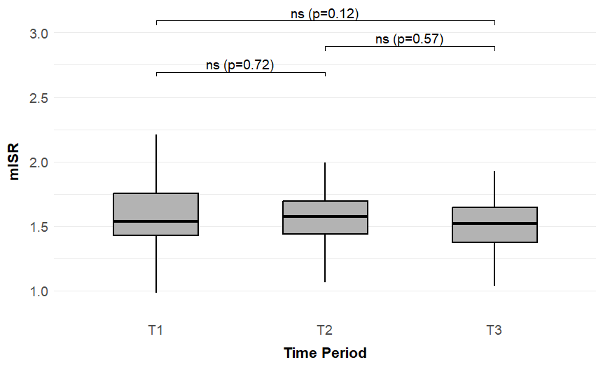
Discussion and conclusions: While a subset of patients with revision UKA to TKA demonstrated notable patellar tendon shortening over time, the overall cohort did not show a clinically meaningful change. Although a significant 3% decrease in the mISR emerged beyond six months, this subtle difference fell below the predefined ≥10% threshold. These findings suggest that while minor changes can occur, their clinical relevance remains uncertain, underscoring the need for further long-term investigation.




