German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Perioperative complications and mid-term outcomes in total hip and knee joint arthroplasty among solid organ transplant recipients: Lowest reoperation-free survival and patient survivorship in lung transplant recipients
Text
Objectives and questions: Performing total joint replacements (TJR) in patients with solid organ transplantations (SOT) is associated with an increased risk of complications and reoperation. The aim of this study is to report on implant survivorship, patient survivorship, and complication rates for total knee arthroplasty (TKA) and total hip arthroplasty (THA) performed in heart, lung, liver and kidney transplant recipients.
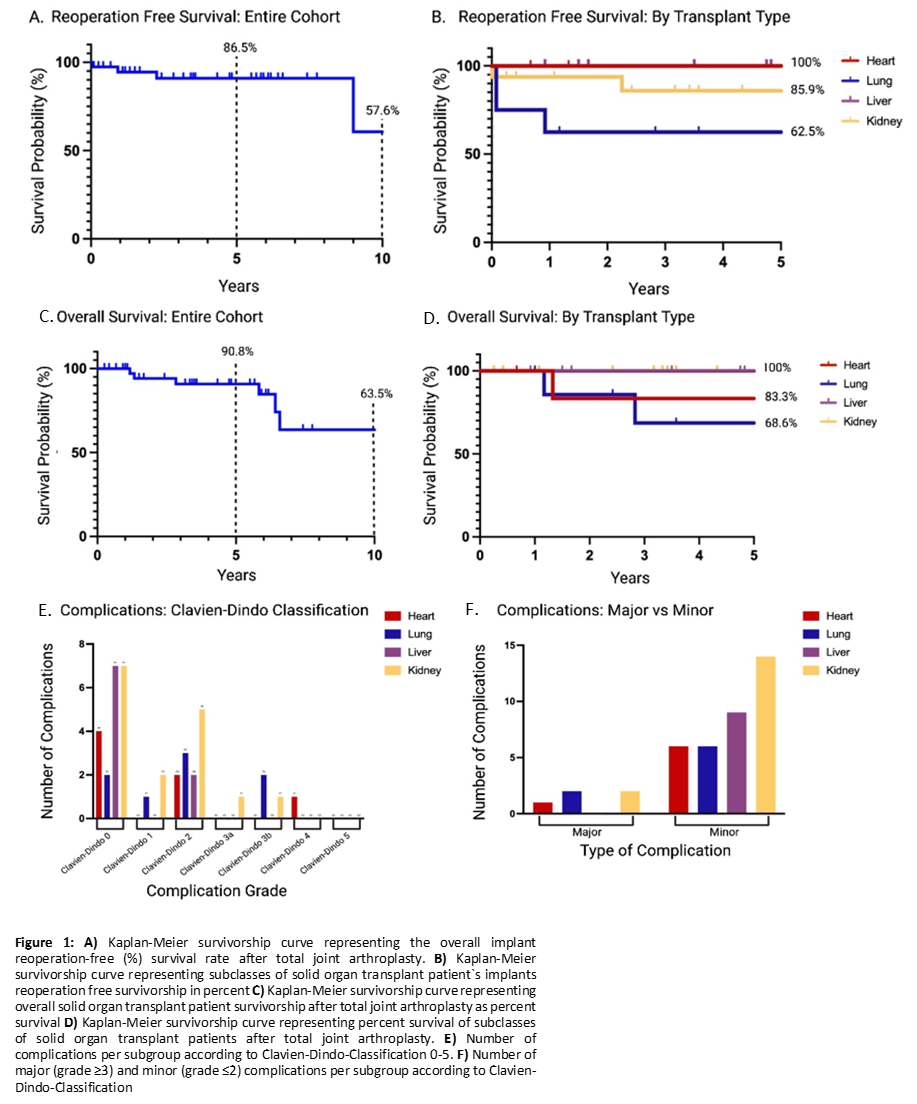
Material and methods: Forty patients with heart, lung, liver, or kidney transplants who underwent primary THA or TKA between January 1, 2013, and July 31, 2023, were included in the retrospective analysis. Implant survivorship, reoperation-free survivorship, patient survivorship, and complication rates were compared between the subgroups. In the analysis of complications across different organ groups, Fisher’s Exact Test was used to assess the distribution of all Clavien-Dindo complication grades (0 to 5), as well as to conduct a separate comparison between major (grade ≥3) and minor (grade ≤2) complications across the organ groups. A P value of <0.05 was considered statistically significant (* p<0.05 , ** p<0.01). Kaplan-Meier survivorship curves were used to demonstrate overall patient survivorship for the entire cohort and the subgroups, as well as re-operation free implant survival for the entire cohort and the organ specific subgroups. Comparisons between groups were tested using a log-rank test.
Results: At a mean follow-up of up of 5.18 years, Implant survivorship and reoperation-free survival for the entire cohort at the last follow-up were 97.5% and 85%, respectively. Kaplan-Meier survival estimates demonstrated 5- and 10-year reoperation-free survival rates of 86.5% (95% CI: 76%–98.4%) and 57.6% (95% CI: 25.6%–100%), respectively. The lung transplant group had the shortest reoperation-free survival, although not statistically significant (p = 0.07), a significantly higher risk of reoperation, with a hazard ratio (HR) of 6.9 (95% CI: 1.1–41.2, p = 0.04) and both the lowest 5-year patient survivorship at 68.6% (p=0.04) and the highest risk of death after TJR with a HR of 7 (95% CI: 1.2–45.5, p=0.03).
Discussion and conclusions: Patients with SOT exhibit excellent mid-term implant survivorship, with a rate of 97.5%. Lung transplant recipients show the lowest rates of both reoperation-free survival and overall patient survivorship compared to heart, kidney, and liver transplant recipients. Despite this, the 90-day complication rates are similar across all organ groups.
Figure 1 [Abb. 1]