German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Statistical shape modelling of the intramedullary femoral canal defines femoral stem orientation
Text
Objectives: Multiple studies have identified a discrepancy between femoral neck version (FNV) and prosthetic femoral version (PFV) after uncemented total hip replacement (THR). Despite this, FNV remains a key parameter/variable considered in three-dimensional (3D) surgical planning. While the proximal femoral canal shape influences femoral component positioning, its morphology is rarely accounted for.
We aimed to better understand the shape features of and differences between the canal and external proximal femur.
Our objectives were to: 1. Build sex-specific statistical shape models (SSMs) on femoral canals and cortices to identify key shape variations; 2. Compare the main anatomical variables between these models.
Material and methods: This single-center retrospective study used 80 (40 male, 40 female) pre-operative pelvic CT scans of osteoarthritic patients who underwent THR. The femoral canal and proximal femur were segmented using medical image processing software.
Each dataset was standardised for length and a standard surgical coordinate system was defined before shape alignment. Four SSMs were built: sex-specific models for both the internal and external anatomy. For each model a point mapping tool aligned each input surface to a computed mean shape.
Principal Component Analysis identified shape variation patterns, described using a finite number of principal components (PCs).
Outcome measures: Cumulative variance captured by the first 5 PCs in each model.
Key anatomical variations identified in each model.
Results: In males, the first 5 PCs explained 85% and 88% of the variance in the femoral canal and proximal femur shape, respectively. In females, the first 5 PCs explained 88% and 92%, respectively.
Common variations in all models included size, torsion (version), varus/valgus alignment, and prominence of the greater trochanter. The external anatomy also revealed changes in the neck shaft angle (NSA) and femoral neck length.
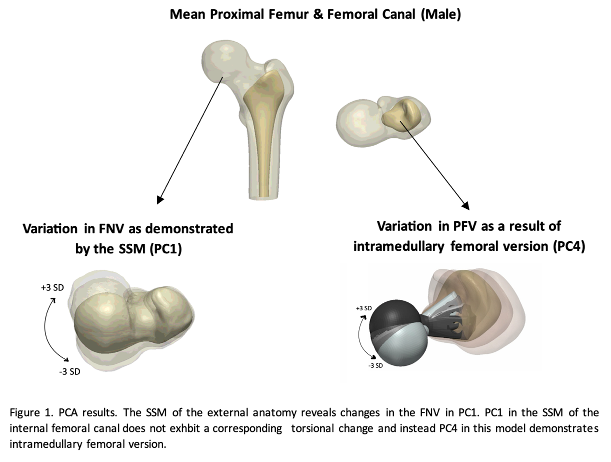
In males, PC1 of the external anatomy SSM showed FNV and varus/valgus changes, while the internal model showed only the latter, suggesting FNV changes do not necessarily reflect intramedullary version changes (Figure 1 [Abb. 1]).
Similarly, in females, PC2 of the external anatomy SSM showed NSA and varus/valgus alignment changes, while the corresponding PC in the internal model revealed torsional changes.
Discussion and conclusions: Surgeons have limited control over femoral stem positioning in uncemented THR, as the canal’s twist and bow guide its final orientation. Our SSMs show the internal and external femoral shapes differ. Key anatomical features include size, torsion and varus/valgus alignment. THR planning should consider these rather than relying solely on FNV.