German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Immunological competence as a critical risk factor for implant-associated infections in hip arthroplasty
Text
Objectives and questions: Implant-associated infections remain a major challenge in hip arthroplasty, particularly among fracture patients, who exhibit higher infection rates than those undergoing elective procedures. This study is the first to explore immune cell distribution and phenotypic variations in hip arthroplasty patients, hypothesizing that differences in immunological competence contribute to the higher infection rates in trauma surgeries compared to elective procedures.
Material and methods: In this prospective study, 30 patients undergoing total hip arthroplasty were enrolled, including 17 with osteoarthritis and 13 with femoral neck fractures. Fracture patients were older (82.1 ± 11.2 vs. 69.1 ± 11.4 years) with higher leukocytes (12.3 ± 7.9 vs. 7.3 ± 2.2 cells/nl) and C-reactive protein levels (30.6 ± 29.5 vs. 2.6 ± 1.59 mg/L), while BMI was similar (24.5 ± 3.3 vs. 26.0 ± 4.1 kg/m²). Peripheral blood samples were collected preoperatively (D0) and on postoperative days 1, 3, and 7. Flow cytometry was employed to assess immune cell populations, including granulocytes (CD19⁺, CD56⁺), monocytes (CD14⁺), various T-helper subsets (Th1, Th2, Th9, Th17, Th22), and regulatory T cells (CD25⁺, CD127⁻). Paired t-tests were used to compare immune cell distributions over time, with statistical significance set at *p < 0.05, **p < 0.01, ***p < 0.001.
Results: Preoperative analysis revealed significant differences between the osteoarthritis and fracture groups, with fracture patients showing marked shifts in eosinophils, B cells, cytotoxic T cells, and T-helper cells. Postoperatively, the fracture group exhibited significant alterations in basophil and eosinophil counts on day 1, and sustained differences in natural killer and mast cell populations on days 3 and 7 (Figure 1 [Abb. 1]). These findings indicate that fracture patients have distinct pre- and postoperative immune profiles that may predispose them to an increased risk of implant-associated infections.
Figure 1: Kinetics of Immune Cell Distribution in Hip Osteoarthritis and Fracture Patients. Immune profiling of hip osteoarthritis and fracture patients at time points (pre-surgery: D0, post-surgery: D1, D3, D7) in peripheral blood, as percentages of CD45+ cells. Data are mean ± SEM.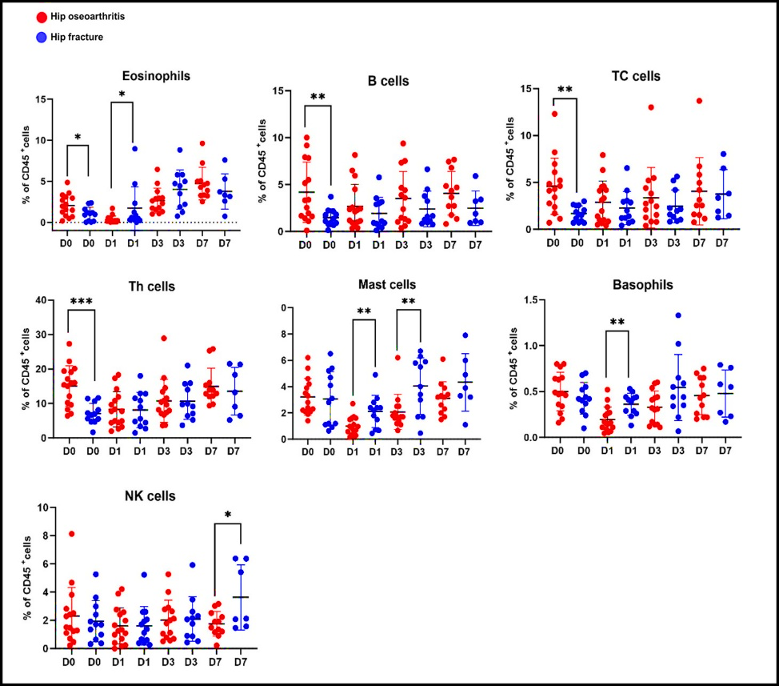
Discussion and conclusions: This is the first study to demonstrate that inherent differences in immunological competence, particularly in granulocyte and T-cell subsets, may underlie the higher incidence of implant-associated infections in trauma patients. These results provide novel insights into the role of the immune system in postoperative infection susceptibility following hip arthroplasty and suggest that preoperative immune profiling could be instrumental in risk assessment and the development of tailored clinical interventions.




