German Congress of Orthopaedics and Traumatology (DKOU 2025)
Deutscher Kongress für Orthopädie und Unfallchirurgie 2025 (DKOU 2025)
Unilateral lumbo-pelvic fixation for unilateral sacral fracture: A finite element analysis
Text
Objectives and questions: Unilateral sacral fractures with posterior ring instability represent a prevalent type of posterior pelvic ring fracture. While lumbo-pelvic fixation is recognized as a highly stable method, the sufficiency of unilateral lumbo-pelvic fixation (ULF) for such fractures remains under debate. This study aims to assess the biomechanical stability of ULF compared to traditional bilateral lumbo-pelvic fixation (BLF) and triangular osteosynthesis (TO), incorporating clinical observations and previous biomechanical data.
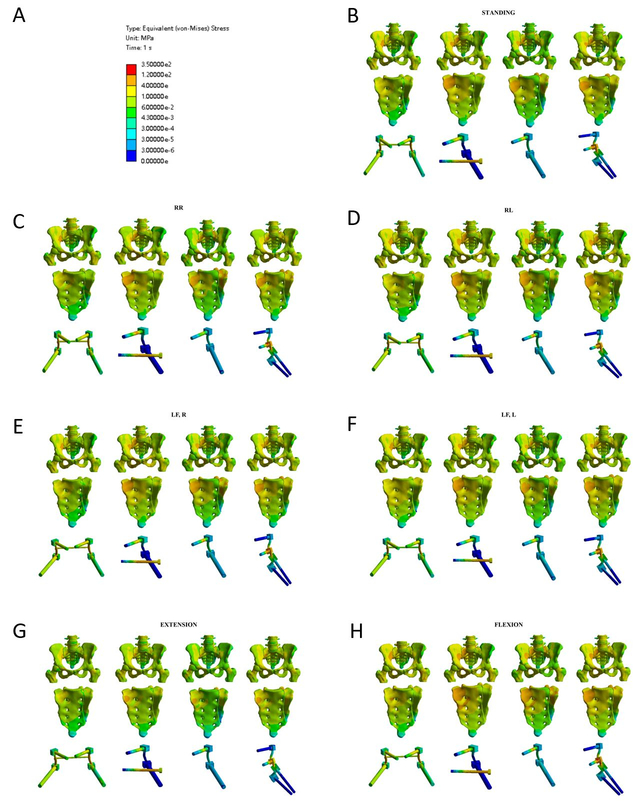
Material and methods: A three-dimensional finite element model of the spine-pelvis complex was developed using CT data from a healthy male volunteer. The model included lumbar vertebrae, sacrum, pelvis and femur with a simulated unilateral sacral fracture (AO C1.3) created by introducing a 0.5 mm gap on the left sacral side. Unilateral lumbo-pelvic fixation with two screws (2ULF), four screws (4ULF), triangular osteosynthesis (TO) and bilateral lumbo-pelvic fixation (BLF) were designed in SolidWorks and analyzed in ANSYS. Material properties for cortical and trabecular bones were assigned based on physiological data and ligaments were modeled using spring-damper elements. The constructs were subjected to physiological loading conditions, including a 600 N downward force and a 10 Nm torque, to simulate movements such as flexion, extension and lateral bending. Fracture displacement and stress distribution were evaluated across models and the results were validated against published biomechanical data.
Results: Our findings indicate that BLF and TO provide greater stability than ULF, with BLF emerging as the most stable model. While ULF may be insufficient for immediate postoperative weight-bearing, TO also demonstrated potential risks of instability during rotational and lateral bending movements toward the fracture side.
Discussion and conclusions: Despite its application in clinical settings, ULF may not adequately support early postoperative mobility. This study underscores the need for cautious application of ULF and suggests that enhancements such as additional fixation points may be necessary. The results also highlight the importance of tailored postoperative rehabilitation strategies for patients undergoing TO, especially in managing movements that could destabilize the fracture site.
Figure 1 [Abb. 1]
Figure 1: Stress distribution diagrams of four internal fixation methods under seven different postures. For each column, the figures from top to bottom represent: overall stress, sacral stress, and internal fixation stress. A: color scale representing von-Mises stress distribution B: standing posture C: rotation to the right D: rotation to the left E: lateral flexion to the right F: lateral flexion to the left; G: extension H:flexion