Deutscher Rheumatologiekongress 2025
Deutscher Rheumatologiekongress 2025
Fluctuating changes in T cells during pregnancy in Systemic Lupus Erythematosus
Text
Introduction: Systemic lupus erythematosus (SLE) poses unique and significant challenges during pregnancy, primarily due to its association with a high prevalence of maternal and fetal complications, including disease flares, preeclampsia, and adverse pregnancy outcomes [1]. Despite advances in understanding autoimmune diseases, the precise interplay between the immunological adaptations necessary for maintaining pregnancy and the pathophysiological mechanisms of SLE that contribute to disease exacerbation remains poorly understood. This study intends to analyze the dynamics of T-helper (Th) subgroups in SLE patients across the course of pregnancy and the postpartum period, providing insights into their potential roles in modulating immune responses during gestation.
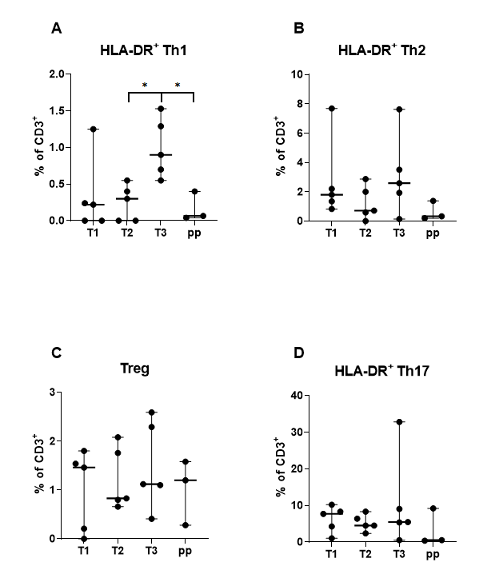
Methods: A single-center prospective cohort study was carried out, including seven SLE patients treated at our clinic between January 2022 and April 2023. Peripheral blood samples were collected from seven SLE pregnancies during each trimester (T1, T2, T3) and the postpartum period (pp). Th1, Th2, Th17 and Treg were analyzed using flow cytometry, and statistical evaluation was performed using the Mann-Whitney test.
Results: We identified a significant increase in proinflammatory activated Th1-cells during the third trimester compared to the second semester followed by a decrease postpartum. While activated Th2 cells exhibited similar fluctuations, these changes were not statistically significant. Activated Th2 and Treg display a decline from the first to the second trimester, however activated Th2 cells decrease postpartum while Treg increase till the postpartum period. Activated Th17 cells remained stable throughout pregnancy but decreased after delivery.
Conclusion: Given that SLE is classified as a Th2-dominant condition and pregnancy is associated with a physiological increase in Th2 cell levels, this could potentially contribute to disease flares during gestation. However, the small size of this cohort limits definitive conclusions regarding the relationship between immunological shifts and disease activity. Further analysis in a larger sample is warranted.
Disclosures: VR: Eli Lilly, JH: ABVVIE, Astra-Zeneca, GSK, Janssen, Novartis, UCB, RK: None declared, ACP: None declared.
Figure 1 [Fig. 1]
Figure 1: T-helper subgroups in pregnant women with Systemic Lupus erythematosus. The Th1-cells increase significantly from the second to the third trimester and show a significant decrease postpartum. (A) Activated Th1-cells. (B) Activated Th2-cells. (C) T-regulatory cells. (D) Activated Th17-cells. Statistically significant results *p = < 0,05. Abbreviations: HLA-DR, Human Leukocyte Antigen – DR isotype; Th, T-helper cell; Treg, T-regulatory cell; T, Trimester; pp, postpartum.