Deutscher Rheumatologiekongress 2025
Deutscher Rheumatologiekongress 2025
Elevated type I interferon activity in primary APS patients with thrombocytopenia
Text
Introduction: Antiphospholipid syndrome (APS) is a systemic autoimmune disorder primarily characterized by thrombotic events and/or obstetric complications, in the presence of persistent antiphospholipid antibodies. Thrombocytopenia was recently incorporated into the 2023 revised ACR/EULAR criteria for APS [1]. Type I interferon (IFN) upregulation has been identified as a potential contributor to clinical disease in a subset of APS patients [2]. However, the relationship between type I IFN and thrombocytopenia in this population has yet to be further delineated.
The primary objective of this study was to investigate a possible association between thrombocytopenia and elevated type I IFN in APS patients.
Methods: A retrospective analysis was conducted among 211 APS patients seen in our department between 2017 and 2024. Clinical manifestations, with a particular focus on thrombocytopenia, and laboratory characteristics (specifically autoantibody profiles and SIGLEC-1 expression on monocytes as a surrogate marker for elevated type I IFN [3]) were evaluated. The relationship between type I IFN, thrombocytopenia, and other disease manifestations was assessed using the Mann-Whitney U test and Spearman’s correlation for statistical analysis.
Results: Among the 211 APS patients, 56 were identified as having experienced thrombocytopenia during the observational period (20 with primary APS and 36 with secondary APS associated with systemic lupus erythematosus (SLE)). APS patients with thrombocytopenia exhibited higher SIGLEC-1 expression levels on monocytes compared to those without thrombocytopenia, with an inverse correlation observed between platelet count and SIGLEC-1 expression (Figure 1A[Fig. 1]). Additionally, thrombocytopenic patients showed elevated levels of anti-Cardiolipin IgG antibodies (p = 0.0039) and a trend towards increased anti-β2-Glycoprotein IgG antibodies (p = 0.051). Notably, the enhanced type I IFN signature was significant only in primary APS patients with thrombocytopenia (Figure 1B[Fig. 1]), with no significant difference observed in the secondary APS cohort (Figure 1C[Fig. 1]). APS patients with thrombocytopenia also demonstrated a higher overall disease burden, with distinct clinical presentations between primary and secondary APS. In comparison to non-thrombocytopenic patients, primary APS patients with thrombocytopenia exhibited a higher incidence of venous thromboembolic events (55% vs. 35.48%) and a lower occurrence rate of arterial events (15% vs. 29%). In contrast, secondary APS patients with thrombocytopenia experienced a greater frequency of mixed venous and arterial events (27.78% vs. 12.9%) as well as obstetric complications (19.44% vs. 17.74%).
Figure 1: (A) Siglec-1 values relecting type I IFN were compared between APS patients with thrombocytopenia and without thrombocytopenia Mean with SEM, Mann-Whitney test.; Correlation of platelet number and Siglec-1 values in APS patients Spearman correlation. Created with GraphPad Prism 9. (B) Comparison of Siglec-1 expression between primary APS patients with thrombocytopenia and without thrombocytopenia Mean with SEM, Mann-Whitney test. (C) Siglec-1 expression levels of secondary APS patients with thrombocytopenia versus those without thrombocytopenia Mean with SEM, Mann-Whitney test. * for p<0,05; ** for p<0,01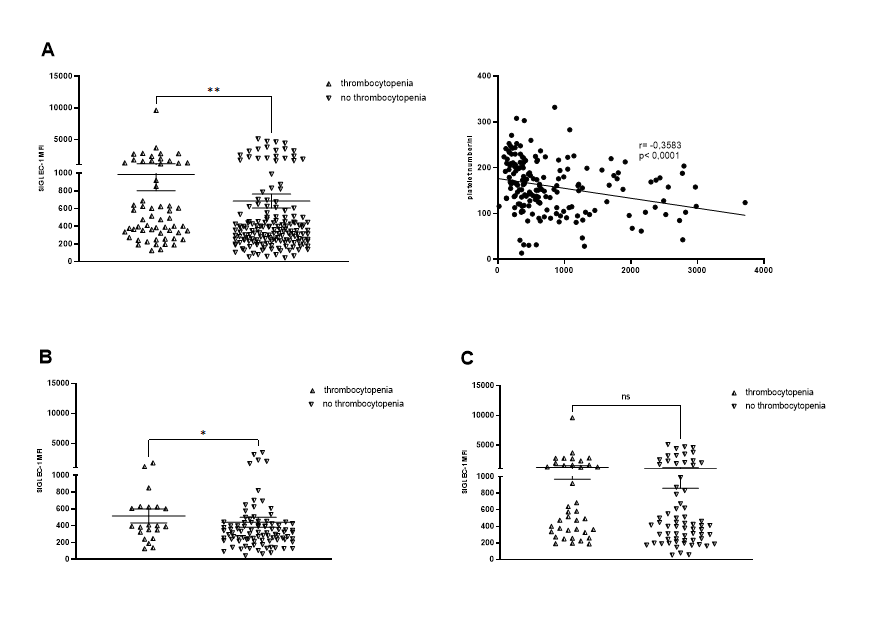
Conclusion: The data suggest that type I IFN may play a key pathogenic role in thrombocytopenia in primary APS. Furthermore, APS patients with thrombocytopenia exhibit higher autoantibody profiles and more severe disease manifestations, particularly in relation to thromboembolic and obstetric complications. These findings warrant confirmation in prospective studies and could inform the development of targeted therapeutic strategies for APS.
Literatur
[1] Barbhaiya M, Zuily S, Naden R, Hendry A, Manneville F, Amigo MC, Amoura Z, Andrade D, Andreoli L, Artim-Esen B, Atsumi T, Avcin T, Belmont HM, Bertolaccini ML, Branch DW, Carvalheiras G, Casini A, Cervera R, Cohen H, Costedoat-Chalumeau N, Crowther M, de Jesus G, Delluc A, Desai S, De Sancho M, Devreese KM, Diz-Kucukkaya R, Duarte-Garcia A, Frances C, Garcia D, Gris JC, Jordan N, Leaf RK, Kello N, Knight JS, Laskin C, Lee AI, Legault K, Levine SR, Levy RA, Limper M, Lockshin MD, Mayer-Pickel K, Musial J, Meroni PL, Orsolini G, Ortel TL, Pengo V, Petri M, Pons-Estel G, Gomez-Puerta JA, Raimboug Q, Roubey R, Sanna G, Seshan SV, Sciascia S, Tektonidou MG, Tincani A, Wahl D, Willis R, Yelnik C, Zuily C, Guillemin F, Costenbader K, Erkan D; ACR/EULAR APS Classification Criteria Collaborators. The 2023 ACR/EULAR Antiphospholipid Syndrome Classification Criteria. Arthritis Rheumatol. 2023 Oct;75(10):1687-702. DOI: 10.1002/art.42624[2] Xourgia E, Tektonidou MG. Type I interferon gene expression in antiphospholipid syndrome: Pathogenetic, clinical and therapeutic implications. J Autoimmun. 2019 Nov;104:102311. DOI: 10.1016/j.jaut.2019.102311
[3] Biesen R, Demir C, Barkhudarova F, Grün JR, Steinbrich-Zöllner M, Backhaus M, Häupl T, Rudwaleit M, Riemekasten G, Radbruch A, Hiepe F, Burmester GR, Grützkau A. Sialic acid-binding Ig-like lectin 1 expression in inflammatory and resident monocytes is a potential biomarker for monitoring disease activity and success of therapy in systemic lupus erythematosus. Arthritis Rheum. 2008 Apr;58(4):1136-45. DOI: 10.1002/art.23404




