32. Jahrestagung der Gesellschaft für Arzneimittelanwendungsforschung und Arzneimittelepidemiologie (GAA)
32. Jahrestagung der Gesellschaft für Arzneimittelanwendungsforschung und Arzneimittelepidemiologie (GAA)
Das individuelle Pharmakotherapie-Management (IPM) mit definierten elektronischen Patienten- und Medikamenten-Scores verhindert weitreichende multidimensionale Risiken der Polypharmazie und ist mit KI-Unterstützung universell einsetzbar
Text
Background: In multimorbidity and severe acute critical illness, polypharmacy [1] is mostly unavoidable. There is no prevention tool that considers the full range of risks [2] associated with adverse drug reactions (ADRs), intensified by drug-drug interactions (DDIs), drug-disease interactions (DDSIs), incorrect dosing and contraindications for the individual patient condition. An AI-based version would provide high future impact and is urgently needed. This study addressed these ongoing high-risk, high-consequence challenges for vulnerable patient groups in geriatric traumatology, intensive care, and transplantation medicine [3], [4] at University Medicine Halle (UMH) to provide and evaluate an evidence-based digital drug therapy and patient safety concept.
Materials and Methods: Real-world challenges in the half-daily routine reviewing of 25 to 52 high-risk polypharmacy medications, meanwhile 68,500 self-conducted medication reviews, necessitated a standardised, personalised bottom-up design to prevent any drug-related risks in polypharmacy. The Individual Pharmacotherapy Management (IPM) approach was conceptualised by applying defined patient scores based on individual patient conditions from his/her electronic health records, including diagnoses, laboratory data on organ functions and vital parameters and referring to the SmPCs for each individual medication adaption (Figure 1 [Fig. 1]). The associated effectiveness of IPM was assessed using retrospective pre/post studies in geriatric traumatology [5] on the primary outcomes of delirium, in-hospital falls, and renal impairment, with multivariable regression analyses. Furthermore, IPM efficiency was analysed based on comparative internal hospital quality control data in interdisciplinary intensive care units (ICU).
Figure 1: Comprehensive, reproducible Individual Pharmacotherapy Management to identify and counteract individual pathophysiological patient conditions which may be iatrogenically induced by drugs. 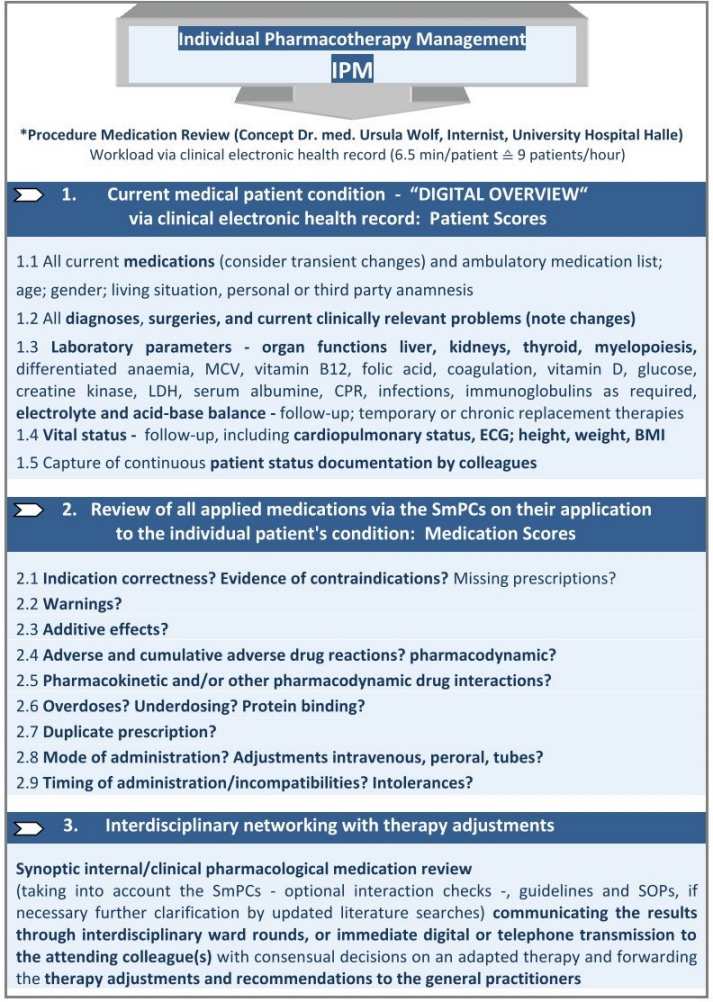
* IPM (applied Patient and Medication Scores) based on the inpatient Electronic Health Record (EHR) and Summaries of Product Characteristics (SmPCs), defined, conceptualised, implemented and practised by Ursula Wolf, MD, Head of Pharmacotherapy Management Department, Specialist in Internal Medicine with expertise in Clinical Pharmacology, performed >65,800 individual medication reviews for polypharmacy in elderly trauma, dementia, transplant and intensive care patients. The IPM physician applies the SmPCs by matching their evidence-based defined risks to the digitally captured individual Patient Scores which provide the necessary ‘comprehensive patient overview’.
Results: The resulting IPM medication adaptions primarily related to identified pathophysiological abnormalities from cumulative ADRs, frequently pharmacodynamic DDIs, overdoses, pharmacokinetic DDIs, DDSIs, contraindications, anticholinergic burden, high-risk psychotropic drugs, benzodiazepines, serotonergic opioids, and missing prescriptions. The resulting targeted, personalised IPM interventions were associated with multidimensional, significant reductions of delirium (90 rel%), in-hospital falls (83 rel%) and any progression of renal impairment (100 rel%), identifying associated risk factors. The average length of stay for the most severely ill ICU patients decreased from 29.1 to 23.2 days within four years from onset of the IPM implementation. This provided a higher capacity for patients to be treated, by 32.7% in the ICUs, where critically ill patients are often mechanically ventilated and dialysed. Despite higher patient numbers, medication costs in the two interdisciplinary ICUs reduced by €451.597 (28%) during the first four IPM-years already [5], [6], [7], [8]. Drawing on her experience of conducting over 68,500 IPM analyses, the author has also approved the applicability of AI-assisted IPM with simulated models. This is achieved by continuously improving Perplexity-AI, among others, which enables the extended, easy and universal use of IPM. This application is accessible not only to healthcare providers, but to everyone, and supports patient empowerment, co-responsibility and health literacy. In patient care, anonymised, AI-supported IPM requires informed consent from the patient. Only the attending physician is authorised to implement IPM therapy recommendations.
Conclusion: According to the IPM real-world evidenced multidimensional preventive associations, the use of IPM scores ensures effective reproducibility and interoperability, even in multiprofessional teams and AI-supported applications. This structured, methodical strength and robustness positions the IPM as an internationally applicable model for improving drug therapy and patient safety in polypharmacy and caring for vulnerable patient groups, contributing to the running WHO-coordinated UN Decade of Healthy Ageing (2021-2030) [9].
Literatur
[1] World Health Organization. Medication Safety in Polypharmacy. WHO/UHC/SDS/2019.11. Geneva: WHO; 2019. Available from: https://www.who.int/docs/default-source/patient-safety/who-uhc-sds-2019-11-eng.pdf[2] Wolf U, Eckert S, Walter G, Wienke A, Bartel S, Plontke SK, Naumann C. Prevalence of oropharyngeal dysphagia in geriatric patients and real-life associations with diseases and drugs. Sci Rep. 2021;11:21955. DOI: 10.1038/s41598-021-99858-w
[3] Wolf U. A Drug Safety Concept (I) to Avoid Polypharmacy Risks in Transplantation by Individual Pharmacotherapy Management in Therapeutic Drug Monitoring of Immunosuppressants. Pharmaceutics. 2023 Sep 10;15(9):2300. DOI: 10.3390/pharmaceutics15092300
[4] Wolf U. A Drug Safety Briefing (II) in Transplantation from Real-World Individual Pharmacotherapy Management to Prevent Patient and Graft from Polypharmacy Risks at the Very Earliest Stage. Pharmaceuticals (Basel). 2024;17(3):294. DOI: 10.3390/ph17030294
[5] Wolf U, Drewas L, Ghadir H, et al. Individual Pharmacotherapy Management (IPM-II) for Patient and Drug Safety in Polypharmacy via Clinical Electronic Health Record Is Associated with Significant Fall Prevention. Pharmaceuticals (Basel). 2024;17(12):1587. DOI: 10.3390/ph17121587
[6] Drewas L, Ghadir H, Neef R, Delank KS, Wolf U. Individual Pharmacotherapy Management (IPM) - I: a group-matched retrospective controlled clinical study on prevention of complicating delirium in the elderly trauma patients and identification of associated factors. BMC Geriatr. 2022;22(1):29. DOI: 10.1186/s12877-021-02630-y
[7] Wolf U, Ghadir H, Drewas L, Neef R. Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III). J Clin Med. 2023;12(13):4545. DOI: 10.3390/jcm12134545
[8] Wolf U, Baust H, Neef R, Steinke T. Individual Pharmacotherapy Management (IPM)-IV: Optimized Usage of Approved Antimicrobials Addressing Under-Recognized Adverse Drug Reactions and Drug-Drug Interactions in Polypharmacy. Antibiotics (Basel). 2022;11(10):1381. DOI: 10.3390/antibiotics11101381
[9] UN General Assembly (75th sess.: 2020-2021). United Nations Decade of Healthy Ageing (2021-2030): resolution / adopted by the General Assembly. A/RES/75/131. Issued in GAOR, 75th sess., Suppl. no. 49. New York: United Nations; 2020 Dec 21 [accessed 2025 Sep 12]. Available from: https://digitallibrary.un.org/record/3895802?v=pdf




