32. Jahrestagung der Gesellschaft für Arzneimittelanwendungsforschung und Arzneimittelepidemiologie (GAA)
32. Jahrestagung der Gesellschaft für Arzneimittelanwendungsforschung und Arzneimittelepidemiologie (GAA)
Individuelles Pharmakotherapie-Management (IPM) identifiziert auch Leitlinien-assoziierte Risiken für die Arzneimitteltherapie- und Patientensicherheit
Text
Background: The Individual Pharmacotherapy Management (IPM) systematically identifies and rectifies drug-related risks, including those arising from guideline-based recommendations, to enhance patient safety [1], [2], [3], [4], [5], [6]. Although clinical practice guidelines lack legal force, they are evidence-based, consensus-driven standards that shape diagnostic and therapeutic decision-making in routine care. Given the importance of drug therapy safety, it is long overdue that the issue of reconciling guideline adherence with patient-centred risk evaluation is addressed.
Materials and Methods: The defining feature of the IPM, conceptualised by the author based on her internal medicine and clinical pharmacology background, is the adaptation of medication scores to patient scores (Figure 1 [Fig. 1]). Drawing on her experience of conducting over 68,500 IPM analyses, the author has also approved the use of AI-assisted IPM with simulated models. In patient care, anonymised, AI-supported IPM requires informed patient consent. The IPM aims to review the medication list as accurately as possible in reference to the individual patient's condition. This uncovers real-world pathophysiological abnormalities and risk factors, particularly in the context of polypharmacy. The resulting personalised evaluation, aligned with guideline recommendations, supports the comprehensive detection of clinically relevant medication risks in the individual patient.
Figure 1: Comprehensive, reproducible Individual Pharmacotherapy Management to identify and counteract individual pathophysiological patient conditions which may be iatrogenically induced by drugs. 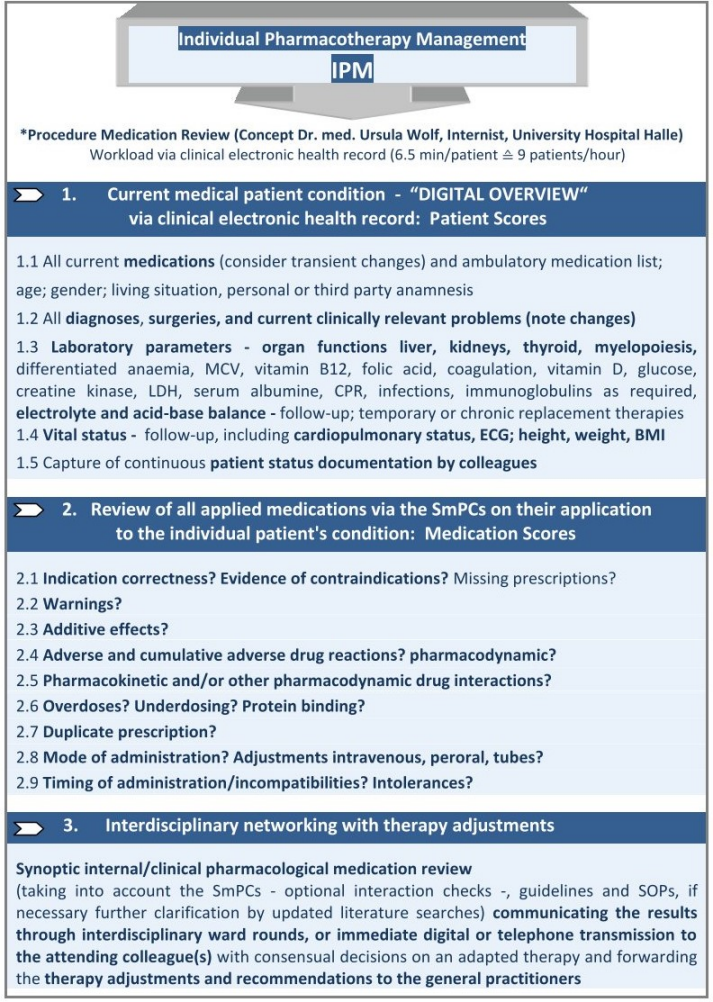
* IPM (applied Patient and Medication Scores) based on the inpatient Electronic Health Record (EHR) and Summaries of Product Characteristics (SmPCs), defined, conceptualised, implemented and practised by Ursula Wolf, MD, Head of Pharmacotherapy Management Department, Specialist in Internal Medicine with expertise in Clinical Pharmacology, performed >65,800 individual medication reviews for polypharmacy in elderly trauma, dementia, transplant and intensive care patients. The IPM physician applies the SmPCs by matching their evidence-based defined risks to the digitally captured individual Patient Scores which provide the necessary ‘comprehensive patient overview’.
Results: IPM also detected risks to drug therapy and patient safety that resulted from guideline-based recommendations. The major categories of risks identified include adverse drug reactions, which can manifest acutely, in the long term or cumulatively. Additional risks arise from over-prescription and drug-disease interactions. It is imperative that these risks are recognised, documented and communicated to the attending physician. While monitoring can reduce certain risks, contraindicated therapies must be strictly avoided in cases of drug-disease interaction. Examples of various contextual IPM-detected cases are presented [7].
Conclusion: In terms of guideline recommendations, it is imperative to eliminate any additional risks to patients that may arise from the recommended drug therapy. Due to the specialization of medical disciplines, comprehensive pharmacological oversight, especially in cases of polypharmacy, is often lacking. Implementing established pharmacological expertise or AI-supported tools such as IPM can serve as effective preventive measures to ensure drug and patient safety in guideline-recommended therapy. Reconciling guideline adherence with patient-centered risk evaluation, IPM offers the unique structured approach to safeguard pharmacotherapy, prevent avoidable harm, and maintain clinical effectiveness.
Literatur
[1] Drewas L, Ghadir H, Neef R, Delank KS, Wolf U. Individual Pharmacotherapy Management (IPM) - I: a group-matched retrospective controlled clinical study on prevention of complicating delirium in the elderly trauma patients and identification of associated factors. BMC Geriatr. 2022;22(1):29. DOI: 10.3390/pharmaceutics15092300[2] Wolf U, Drewas L, Ghadir H, Bauer C, Becherer L, et al. Individual Pharmacotherapy Management (IPM-II) for Patient and Drug Safety in Polypharmacy via Clinical Electronic Health Record Is Associated with Significant Fall Prevention. Pharmaceuticals (Basel). 2024;17(12):1587. DOI: 10.3390/ph17121587
[3] Wolf U, Ghadir H, Drewas L, Neef R. Underdiagnosed CKD in Geriatric Trauma Patients and Potent Prevention of Renal Impairment from Polypharmacy Risks through Individual Pharmacotherapy Management (IPM-III). J Clin Med. 2023;12(13):4545. DOI: 10.3390/jcm12134545
[4] Wolf U, Baust H, Neef R, Steinke T. Individual Pharmacotherapy Management (IPM)-IV: Optimized Usage of Approved Antimicrobials Addressing Under-Recognized Adverse Drug Reactions and Drug-Drug Interactions in Polypharmacy. Antibiotics (Basel). 2022;11(10):1381. DOI: 10.3390/antibiotics11101381
[5] Wolf U. A Drug Safety Concept (I) to Avoid Polypharmacy Risks in Transplantation by Individual Pharmacotherapy Management in Therapeutic Drug Monitoring of Immunosuppressants. Pharmaceutics. 2023;15(9):2300. DOI: 10.3390/pharmaceutics15092300
[6] Wolf U. A Drug Safety Briefing (II) in Transplantation from Real-World Individual Pharmacotherapy Management to Prevent Patient and Graft from Polypharmacy Risks at the Very Earliest Stage. Pharmaceuticals (Basel). 2024;17(3):294. DOI: 10.3390/ph17030294
[7] Wolf U, Wegener M. Proton Pump Inhibitor Prescription in Nursing Home Residents: Prevalence, Appropriateness, and Associated Factors-A Secondary Data Analysis from Three German Regions and the Impact of Guideline Recommendations. Pharmaceuticals (Basel). 2024 Aug 17;17(8):1082. DOI: 10.3390/ph17081082




